Hyperbaric Oxygen Therapy: A Comprehensive Guide to Understanding and Benefits
Hyperbaric Oxygen Therapy (HBOT) is a medical treatment that involves breathing pure oxygen in a pressurized chamber. This therapy has gained popularity due to its diverse applications and promising results across various health conditions.
What is HBOT?
Initially introduced in the mid-20th century, HBOT involves patients inhaling 100% oxygen in a chamber where the atmospheric pressure is increased. This process allows the lungs to gather more oxygen than usual and significantly increases the oxygen levels in the blood, thereby promoting healing and regeneration.
Mechanism of Hyperbaric Oxygen Therapy
HBOT works by increasing the amount of oxygen dissolved in the body’s tissues. Under increased atmospheric pressure, oxygen becomes more soluble in the bloodstream, facilitating its delivery to organs and tissues, even to those with compromised circulation. This heightened oxygen concentration stimulates the release of growth factors and stem cells, accelerating the healing process.
Conditions Treated with HBOT
The therapy has proven effective in treating various conditions such as decompression sickness, non-healing wounds, carbon monoxide poisoning, radiation injuries, and certain infections. Its efficacy in these diverse conditions stems from its ability to promote tissue repair and reduce inflammation.
Procedure and Sessions of Hyperbaric Oxygen Therapy
HBOT sessions typically last from 60 to 90 minutes, with patients comfortably resting inside the pressurized chamber. The number of sessions varies based on the condition being treated and its severity, often ranging from a few to several sessions over weeks or months.
Benefits and Risks of HBOT
The therapy offers numerous benefits, including improved wound healing, reduced swelling, and enhanced recovery from injuries. However, there are some risks associated with HBOT, such as ear injuries, sinus discomfort, and rarely, oxygen toxicity, which are usually mild and transient.
HBOT in Sports and Rehabilitation
Athletes have increasingly adopted HBOT to expedite recovery from injuries and enhance performance. Additionally, it has been utilized in rehabilitation programs, aiding patients in regaining functionality after various medical interventions.
Research and Advancements in HBOT
Ongoing research continues to explore the potential of HBOT in various medical conditions, including neurodegenerative diseases, autism, and chronic conditions, with promising results. Advancements in technology have also led to innovations in the design of hyperbaric chambers, improving patient comfort and efficiency.
Cost and Accessibility of Hyperbaric Oxygen Therapy
The cost of HBOT sessions can vary based on location, facility, and the condition being treated. While accessibility has improved over the years, availability might still be limited in certain regions due to the requirement of specialized equipment and trained personnel.
Myths and Misconceptions about HBOT
Despite its proven efficacy, there are misconceptions surrounding HBOT, such as it being a cure-all or unsafe. Addressing these myths is crucial to help individuals make informed decisions about the therapy.
Patient Experiences and Testimonials
Real-life stories from individuals who have undergone HBOT emphasize its positive impact on their health and quality of life. These testimonials serve as a testament to the therapy’s effectiveness.
Comparing Hyperbaric Oxygen Therapy with Other Treatments
While HBOT offers numerous benefits, it’s essential to compare it with alternative treatments to understand its advantages and limitations fully.
Conclusion
In conclusion, Hyperbaric Oxygen Therapy stands as a promising treatment option across various medical conditions, offering a non-invasive approach to enhance healing and recovery. Its continued research and advancements position it as a valuable component in modern healthcare.
FAQs (Frequently Asked Questions)
- Is HBOT painful or uncomfortable?
- HBOT sessions are generally painless and comfortable, with most individuals experiencing minimal to no discomfort.
- Can anyone undergo HBOT?
- While generally safe, certain medical conditions or medications may contraindicate HBOT. Consultation with a healthcare professional is essential.
- How many sessions of HBOT are typically needed?
- The number of sessions varies based on the condition being treated, and a healthcare provider will determine the appropriate treatment plan.
- Are there any side effects of HBOT?
- Mild side effects like ear popping or temporary vision changes may occur but are usually transient and resolve quickly after the session.
- Is HBOT covered by insurance?
- In some cases, insurance might cover HBOT, especially when it’s prescribed for certain approved medical conditions. However, coverage can vary, and it’s best to check with your insurance provider.
The Interview
Dr. Amir Hadanny joins the podcast to share the positive results of a stroke patient after hyperbaric oxygen therapy.
Highlights:
01:14 About Bill’s Book
03:01 Hyperbaric oxygen therapy with functional MRI
09:24 Brain function and stroke recovery using fMRI
16:53 Neuroplasticity and Hyperbaric oxygen therapy
22:41 Stroke recovery with Dr. Amir Hadanny
Transcript:
Dr. Amir Hadanny 0:00
More interestingly we see that on the right side the so-called healthy side, we saw some mild activation. But after the treatment we see much higher activation, meaning the right hemisphere, the nonaffected hemisphere is being activated when the weak hand is requested to be activated.
Bill 0:26
One second, that’s neuroplasticity happening right there. Right?
Dr. Amir Hadanny 0:32
Exactly this is neuroplasticity right in front of your eyes. So we’re talking about both the injured hemisphere and the noninjured hemisphere. And the reason why we get the other side being affected is the lower image you’re able to see here is the connectivity there is a connection between the injured side and the non-injured side.
Intro 1:00
This is the recovery after stroke podcast with Bill Gasiamis helping you navigate recovery after a stroke.
About Bill’s Book
Bill 1:14
Hello, everyone, it is with great excitement that I share that my book The Unexpected Way That A Stroke Became The Best Thing That Happened is now live and available for sale on Amazon. The links for where to purchase the book will be available in the show notes and the YouTube description. Also, if you go to your local Amazon and type in my name Bill Gasiamis which if that’s too hard, you can also type in Stroke The Best Thing you will see the listing for both the Kindle and the paperback.
Bill 1:46
Thanks so much to everyone who has supported me on this journey and has already purchased a copy. I am very keen to hear your feedback. Now in episode 280, my guest is Dr. Amir Hadanny, who previously joined me on episode 250 titled Hyperbaric Oxygen Therapy, where we discussed the benefits of clinically supervised high-dose hyperbaric oxygen therapy for stroke survivors, even after they had been told that they had reached the plateau and would most likely not recover much more.
Bill 2:25
In today’s episode, we discuss the results of a case study of a 61-year-old male who had a left frontal stroke that caused deficits to the right side, impacting the use of his right hand and the outcome after 60 oxygen therapy sessions, also known as dives. In this episode, Dr. Hadanny takes us through some slides, so if you’d like to see them, you may prefer to watch the interview on YouTube.
Bill 2:56
Dr. Amir. Hadanny, welcome back to the podcast.
Hyperbaric oxygen therapy with functional MRI
Dr. Amir Hadanny 3:01
Thank you so much for having me again. Real pleasure.
Bill 3:04
Thank you for being here. I appreciate it again, we had you on a little while ago on episode 250. And we discussed for the first time, hyperbaric oxygen therapy. We spoke about a few things that your organization and your team have found out there is a way to discover Penumbra is areas of the brain that can be rehabilitated many, many years after the initial 12 to 24 months after stroke.
Bill 3:43
And that you guys have had with oxygen, hyperbaric oxygen therapy, some amazing results in helping stroke survivors improve the deficits and get better in places where they perhaps didn’t think that there was any improvement to be had. At that time, we spoke about what hyperbaric oxygen therapy was and the risks of too much oxygen we spoke about that it’s not necessarily something that can be applied to everybody.
Bill 4:21
Everybody not everybody who comes in for evaluation is a suitable candidate, they may not have the numbers that can be rehabilitated. And the episode I’ve got to say did get quite an interesting response because there are people who are getting hyperbaric oxygen tanks and putting them into their homes and doing their therapy without any real idea. Monitoring guidance or support by anyone from the medical field.
Bill 5:04
So it was a very interesting episode. for that. Here, we’ve got one extreme person, I had a couple of episodes before you on the podcast, who were doing it completely on their own without medical support. And then we’ve got the complete opposite on the other end of the spectrum with hundreds of 1000s of dollars being spent on this, perhaps even more than that. And then how clinics, research studies, and proper evidence-based methods.
Bill 5:42
So what I like about it is that our conversation created the possibility for maybe, maybe other organizations to take on this type of effort so that the science can improve beyond what only, I mean, how Danny and the team are doing. But I love that you’re playing in the game. And recently, I was contacted, because there’s been some updates that we need to share with the audience. Give me a bit of an update as to what you guys have been up to in the last few months.
Dr. Amir Hadanny 6:27
For sure so just to cap on what you just said. So yes, definitely, we talked about the different ways you can apply hyperbaric oxygen therapy, and what I consider hyperbaric oxygen therapy, and what you know, some people called mild hyperbaric oxygen therapy, or mild oxygen. We talked about the issues with safety and efficacy. But, I think there’s a right way to do it, there’s a research backup way to do it.
Dr. Amir Hadanny 7:00
And by all means, I’m opening my arms and hands reaching out, to do more research to prove it much further and further along. We’re just one group that’s leading it, but definitely, people who want to collaborate with us and do more research about it. It’s what the world needs, what the science community needs, and we welcome it.
Dr. Amir Hadanny 7:36
Building on that, we did a nice methods exploration, that I want to report to you guys, on a patient on a stroke patient that we wanted to see what we’re able to achieve with hyperbaric oxygen therapy but measure it on a different way than what we did so far. And the way we did it is with functional MRI. What is functional MRI, I’m sure that most of the viewers know that an MRI or Magnetic resonance imaging machine is that huge donut that you go in, very similar to a CT scan, but makes those weird noises for 30 or 40 minutes.
Dr. Amir Hadanny 8:27
And what you get is great high-resolution images of your brain. But you’re able to build on it by doing a task, meaning I’m asking the patient who’s lying in there to do something, sometimes they watch a screen and do something cognitive. But in this case, he was watching a screen and we gave him buttons. So he’s able to click with his hands on buttons on each hand. And he’s supposed to react to what is being told on the screen, click on it now click on it. And he has to do it as fast as possible.
Brain Function and Stroke Recovery Using fMRI
Dr. Amir Hadanny 9:15
With his hands, what we’re able to do with this technique, one, we’re able to see how quick is meaning the response time. But more interesting, we can see what regions of the brain are being activated and the network that’s processing this activity. And that brings a whole new aspect of research of what you’re able to determine from that. So that’s what we did.
Bill 9:46
So let’s break it down for a second. So you’ve got a patient they have qualified for hyperbaric oxygen therapy. Firstly, they are a stroke survivor. Yep. And the patient goes into The tube. Normally, when we go into the tube of the MRI, we’re not meant to do anything because if we move, we interfere with the signal or the image. And then it has to start again. This particular version of functional MRI is specifically designed to see somebody who is doing an activity so that we can see the before and after.
Bill 10:27
So how their brain looks before the activity begins. And then what happens after the activity begins? So we can see which part of the brain is being used or, or firing, to enable not firing or not firing, so that we’re trying to understand the before and after here.
Dr. Amir Hadanny 10:49
Correct exactly that it’s literally to understand brain function. So not brain anatomy, but function. It’s another tool to access it and a pretty amazing tool. I want to show you so to answer your first question, we’re going to share my screen and hope.
Intro 11:13
If you’ve had a stroke, and you’re in recovery, you’ll know what a scary and confusing time it can be, you’re likely to have a lot of questions going through your mind, like how long will it take to recover? Will I recover? What things should I avoid? In case I make matters worse, doctors will explain things. But, if you’ve never had a stroke before, you probably don’t know what questions to ask.
Intro 11:37
If this is you, you may be missing out on doing things that could help speed up your recovery. If you’re finding yourself in that situation, stop worrying, and head to recoveryafterstroke.com where you can download a guide that will help you it’s called Seven Questions to Ask Your Doctor about your Stroke.
Intro 11:56
These seven questions are the ones Bill wished he’d asked when he was recovering from a stroke, they’ll not only help you better understand your condition, they’ll help you take a more active role in your recovery, head to the website. Now, recoverafterstroke.com and download the guide. It’s free.
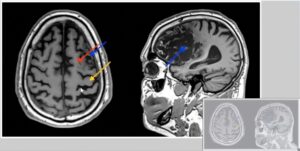
Dr. Amir Hadanny 12:16
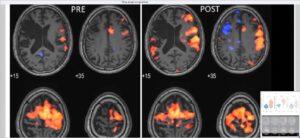
So this is the patient. In our case report that we have published in the scientific literature. This is a 61-year-old male who suffered a left frontal throat, meaning this part of the brain, the left side, about two years, so 24 months before that he was he came to us for hyperbaric oxygen therapy. And what you see here on the right side is you see the destruction or the injury from the stroke, you see all that area that was significantly injured by that left frontal stroke. And so that’s, that’s how we start.
Dr. Amir Hadanny 13:04
That’s the anatomy. And that’s what MRI gives us on the anatomy, those things that we describe here is we talk about where’s the motor cortex, where’s the supplementary motor areas in our brain that are participating in motor function in on those areas, what you see on the on those arrows, stroke was there. But we still don’t have destruction. So the anatomy is still not destroyed.
Dr. Amir Hadanny 13:41
That’s why when we talked about it on the first episode we did together, it’s important to understand who is eligible and who’s not if we have enough to work on that number that you mentioned. So this is what we’re describing here on the left side on the anatomic side. Then, this is what we’re doing. So again, this is a patient that 61 years a 61-year-old person stroke survivor who was treated with 60 sessions and 60 daily sessions.
Dr. Amir Hadanny 14:21
What we see here on the left side is the functional MRI test at baseline, again two years after the stroke when he just started before his first session, and on the right side, we see the brain activation three weeks from when he finished his 60s Diving sessions. What we’re able to see here is it’s pretty convenient to see that with those colors you see exactly which part of his brain is activated, when he’s asked to press the button with the weekend, we have a weekend because of hemiparesis from the stroke.
Dr. Amir Hadanny 15:18
And, please don’t, and maybe for the more sophisticated viewers, here, it seems like the stroke is on the right side, it’s still the left side, it’s just conventions of how fMRI is being shown compared to anatomical MRI, it’s still left frontal, so the right hand was weak. And here’s what we can see at baseline. So basically, no activation at all, in the areas of the motor cortex and the supplementary motor areas on the left hemisphere.
Neuroplasticity and Hyperbaric oxygen therapy
Dr. Amir Hadanny 15:59
And then you see here, those red areas here are exactly that, though, that’s the motor cortex and supplementary motor areas that have been have awoken, meaning we awoke the penumbra, we can get activations in these areas that did not function before. More interestingly, we see that on the right side, the so-called healthy side, we saw some mild activation. But after the treatment, we see much higher activation, meaning the right hemisphere, the nonaffected hemisphere is being activated when the weak hand is requested to be activated.
Bill 16:51
One second, one second. That’s Neuroplasticity. happening right there. Right?
Dr. Amir Hadanny 16:59
Exactly, this is Neuroplasticity right in front of your eyes. So we’re talking about both the injured and the noninjured hemispheres. The reason why we get the other side being affected is the lower image, what you’re able to see here is the connectivity, there is a connection between the injured side and the noninjured side, right hemispheres are connected.
Dr. Amir Hadanny 17:32
So what we’re able to see here is better connectivity between the two hemispheres. And that’s why you’re getting this that’s why you’re getting the higher activation on the non-insured side. So exactly like you said, Neuroplasticity at its best using functional MRI. This correlated with significant improvement of this patient clinically, his weakness has become much stronger as Dougal Meyer went through the roof, sugar Meyer is clinical score, and physical therapists are measuring hand movement after stroke.
Dr. Amir Hadanny 18:14
So significant improvement there, which translated to actual quality of life and daily life activities he was unable to do before. So, this is an incredible case report I wanted to share with you.
Bill 18:30
That is fantastic to see. And, you know, you imagine Neuroplasticity, and people tell you about Neuroplasticity, but it’s this enigma, you can’t see it happening unless there’s an exterior outcome. And if the outcome isn’t dramatic, what people don’t recognize and perhaps don’t give the credit where credit is true. But that’s irrefutable evidence of Neuroplasticity and other parts of the brain.
Bill 19:01
What I call may not be the right word rewiring and recruiting a different part of the brain to support function in an area that was lost in another part of the brain, even though the other, the damaged part is still recovering and being supported by those new the new life that it’s getting through the oxygen therapy where we’ve recruited another part of the brain to get this outcome. It’s amazing.
Bill 19:34
It’s what we get told I got told when I went into rehab about Neuroplasticity, but nobody could show me what it looked like I just was kind of lucky that I had read up on it and knew a little bit about it, and knew that I could activate that on my own through visualization and meditation and being more conscious The aware of my the way that I needed to walk after brain surgery when I wasn’t able to walk.
Bill 20:09
But that’s kind of the missing piece of the puzzle for me. That’s the part that this is what it is, this is the theory behind it. Let me tell you all about it. But now let me show you want Neuroplasticity looks like. So this patient? What’s the next step for that patient? How do they then continue the recovery phase, what happens after they get this outcome at a Viva Aviv clinic?
Dr. Amir Hadanny 20:39
Perfect. So obviously, the road has resurfaced once again. Because this person has been through two years of OT and PT. So we know it’s all about them. But the moment he got to us, you know, that’s, that’s the new baseline. That’s where we are picking it off. And when we can generate Neuroplasticity, we want to capitalize on that, right?
Dr. Amir Hadanny 21:06
So now, we’re pushing him through much, much bigger challenges through more PT and more or to use the new abilities to stimulate more and more new parts of his brain that can generate new functions. So he’s working every day on PT and OT and getting stronger and stronger. Because as you know, you have to get your muscles back, and you need to regenerate those fine movements. Much, much better. So he’s on a new road now. Too much, much better daily life.
Bill 21:48
After 60, 60 dives did you do? Yeah. After 60 Dive, is there a need to do more dives? Would it be more beneficial to continue? I imagine, like a Formula One car at some point, you know, you can spend X amount of time to get the little result and it’s what the insurance companies use as supposedly the excuse that you’ve reached the plateau. So you know, we’ve read he reached the plateau, or this patient reached the plateau, then then the plateau was smashed, and additional recovery was verified, then he’s back into rehab, then is it possible or necessary to continue doing dives?
Stroke recovery with Dr. Amir Hadanny
Dr. Amir Hadanny 22:41
That’s a great question. I can tell you, we don’t know. But the issue is, whatever we gained to gain, those networks that we saw are going to be there, the activations that we saw are going to be there, they’re not going to be lost from not using them or anything. He has built, the rewiring, you mentioned. And that’s not going to go away. The real question is if we wait a while and then do more, another program? Will we gain more?
Dr. Amir Hadanny 23:13
That’s a great question. And this is still something that we’re investigating. The real approach to it is, again, to evaluate to see do we have more Penumbra to work on. Do we think there is more of a number that can react to another one or not? And that’s a great question. Usually most of the improvement and Neuroplasticity, we get on the first program.
Dr. Amir Hadanny 23:41
But Are there cases that can benefit from a second or third one? Yes, there are. But we still don’t have enough to predict which one they are. And we do them on a case-by-case evaluation again, probably he’ll be back to us within a year. We’re going to do the assessment again. Rethink it, do the functional MRI again, and see if we have more to work on or not. Yeah.
Bill 24:11
And who handles the occupational therapy and the physical therapy? Is that done by somebody that you that the clinic collaborates with? Or is it done on his own? Own therapists.
Dr. Amir Hadanny 24:26
So usually when they’re with us during the SR session. It’s all by us. So we have our own PT and our own OT. To be available to them daily hammer it as much as possible, and guide them to do everything. But you know, once they’re out and go back to their daily lives, in most cases, they do not use our guys and go to their own but we They are guidelines and what we want them to do with our recommendation exactly what do they do?
Bill 25:06
Okay, so I understand it’s easier to control the well, it’s not a study, but it’s easier to control the whole process if the therapists are in-house, so to speak, and then they are understanding of what you guys are trying to demonstrate in the study, and how, how to rehabilitate that particular person so that you can then report on, on that in the parameters of how you guys like to get information and deliver information on that.
Bill 25:47
Well, that is fascinating, just as fascinating as it was, when we first spoke in Episode 250. We’ve discussed the next thing that you guys overcame, or dis or found or supported somebody to achieve with oxygen therapy. There are several clinics where you guys have worked, where are you located?
Dr. Amir Hadanny 26:17
We have a couple of clinics. I’m personally at the INR clinic in Central Florida. In the States, we have another one in Asia in Dubai. And our third one is in Israel. And that’s where we do most of our clinical research as well. So right now, though, three clinics are our main ones.
Bill 26:39
Everybody who’s listening, this is an episode that would be awesome. If you happen to go to YouTube and watch it, the links will all be in the show notes go to recoveryafterstroke.com/episodes. You can find out more about the clinic there. I’ll link back to the clinic and also to the YouTube video. And you just need to see those images because a picture tells 1000 words. And it’s really exciting.
Bill 27:07
I get so excited when I see things like that, that I would encourage everybody who’s listening, instead of watching on YouTube to go and have a look. Dr. Amir Hadanny, thank you again for joining us on the podcast.
Dr. Amir Hadanny 27:21
Thank you, Bill. Thank you for having me. Appreciate.
Bill 27:25
Thanks again for joining us on today’s episode. Remember, go to Amazon and type in Bill Gasiamis or stroke the best thing to grab a copy of my book which is available now. You can get it on paper in paperback or you can get it on Kindle. Now if you’re a stroke survivor with a story to share about your stroke experience, come and join me on the show.
Bill 27:49
The interviews are not scripted, you do not have to plan for them. All you need to do to qualify is be a stroke survivor or care for someone who is a stroke survivor. If you are a researcher who wants to share the findings like Dr. Amir of a recent study, you are looking to recruit people into studies You may also wish to reach out and be a guest on my show. If you have a commercial product that you’d like to promote that is related to supporting stroke survivors. To recover there is also a path for you to join me on a sponsored episode of the show.
Bill 28:24
Go to recoveryafterstroke.com/contact and fill out the form explaining briefly which category you belong to. And I will respond with more details about how we can connect via Zoom. Now to all the people who have left a review, thank you so so much it means the world to me.
Bill 28:43
It means that this podcast episode is found easier by more stroke survivors. And what that means is that that helps them on the recovery just like this podcast has helped you on your recovery and made a difference in your life and made you feel like you were less alone or that somebody else out there at least understood what you were going through.
Bill 29:09
That’s what it’s doing for other people who desperately need more information about their stroke recovery journey. So if you’d like to leave a review, but haven’t yet, just go to iTunes or Spotify, and leave a five-star review and a few words about what the show means to you. If you’re watching on YouTube, leave a comment below the video I love receiving them. And I will always respond. And like the episode share the episode, hit the notifications bell.
Bill 29:41
And as always, to learn more about my guests including links to this social media. And to get a full transcript of the entire interview please go to recoveryafterstroke.com/episodes. Thank you once again for listening, being here, and supporting me, I appreciate seeing you on the next episode.
Intro 29:59
Importantly, we present many podcasts designed to give you an insight and understanding into the experiences of other individuals’ opinions and treatment protocols discussed during any podcast or the individual’s own experience and we do not necessarily share the same opinion nor do we recommend any treatment protocol discussed all content on this website. at any linked blog, podcast, or video material controlled this website or content is created and produced for informational purposes only and is largely based on the personal experience of Bill Gasiamis.
Intro 30:33
The content is intended to complement your medical treatment and support healing. It is not intended to be a substitute for professional medical advice and should not be relied on as health advice. The information is general and may not be suitable for your personal injuries, circumstances, or health objectives. Do not use our content as a standalone resource to diagnose, treat, cure, or prevent any disease for therapeutic purposes or as a substitute for the advice of a health professional.
Intro 30:58
Never delay seeking advice or disregard the advice of a medical professional, your doctor, or your rehabilitation program based on our content. If you have any questions or concerns about your health or medical condition, please seek guidance from a doctor or other medical professional if you are experiencing a health emergency or think you might be, call 000 if in Australia or your local emergency number immediately for emergency assistance or go to the nearest hospital emergency department medical information changes constantly.
Intro 31:25
While we aim to provide current quality information in our content. We did not provide any guarantees and assume no legal liability or responsibility for the accuracy, currency, or completeness of the content. If you choose to rely on any information within our content, you do so solely at your own risk. We are careful with the links we provide however third-party links from our website are followed at your own risk and we are not responsible for any information you find there.






