Living with Aphagia after a stroke requires resilience and toughness amongst other things and Alina Gonzales has those qualities in spades. In her time of need, she is also thinking of others and reaching out to raise awareness about stroke.
Highlights:
02:09 Introduction
06:09 Hemorrhagic Stroke Caused By an AVM
12:16 Balancing Between Patience And Impatience
17:28 Loss of Hearing Can Cause Balance Issues
27:32 How Hard Is It For The Caregivers?
39:51 Living with Aphagia
48:23 Continuous Learning
Transcription:
Barbara Gonzales 0:00
Absolutely none when she came home, for some reason, because of COVID. We had no instructions on how to do anything. And she was on a feeding tube, which she still is, but I figured it out.
Barbara Gonzales 0:14
And it was very daunting to come home in a hospital bed with a trach and a feeding tube and not able to communicate, I was told not to bring her home. They wanted her to go to a facility, a long-term facility and I didn’t want that. And I know that she’s thrived as a result of being here. She wouldn’t be as well as she is if she was elsewhere.
Intro 0:46
This is the recovery after stroke podcast with Bill Gasiamis, helping you navigate recovery after a stroke.
Bill Gasiamis 1:34
Hello, and welcome to another episode of the Recovery after Stroke podcast. Recently, Spotify released a new feature that allows people to now rate their favorite shows similarly to how the Apple podcast app allows it.
Bill Gasiamis 1:49
So if you think the show recovery after stroke podcast deserves it, I’d love it if you leave it a five-star review. This will help the show rank better on search engines to help newly diagnosed stroke survivors and their carers find the show and it could make a massive difference in their recovery.
Introduction – Living with Aphagia

Bill Gasiamis 2:09
So go to your favorite podcast app and share what the podcast means for you. It really will make a huge difference. And I will appreciate it. Now this is episode 185 And my guest today is Alina Gonzalez, who experienced bleeding in the brain at the age of 40 that was caused by an arteriovenous malformation or an AVM.
Bill Gasiamis 2:34
When she reached out to connect with me via Instagram messenger, this is what Elena wrote. Hi, Bill, I want to help. I’m 16 months post-event. How can I be useful? Thank you, Alina.
Bill Gasiamis 2:50
It was an impressive first introduction. Of course, the messenger doesn’t reveal the extent of how the stroke has impacted my guests. So I’m always impressed when I turn up and move heaven and earth to be on the other side of the Zoom call.
Bill Gasiamis 3:07
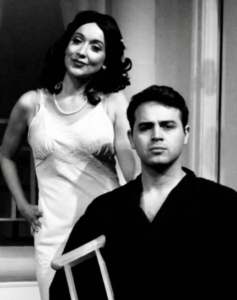
This was no different. Assisting in this interview is Alina’s mum who is sitting out of frame for much of the podcast, and I refer to her as mum for the majority of the interview.
Bill Gasiamis 3:20
But she does appear at the end of the episode where we finally get to see her face and learn her name. Alina has vocal chord issues that she is working hard on rehabilitating and also experiences difficulties with balance among other things.
Bill Gasiamis 3:37
So listen intensely because what she shares is sure to be useful to your stroke recovery. Alina Gonzalez, welcome to the podcast.
Alina Gonzales 3:48
Hi, how are you?
Bill Gasiamis 3:51
I’m well, it was a bit of a struggle for you to get to this meeting. You’ve missed it a couple of times. And today you’re running a little bit late you finally got here. How are you?
Alina Gonzales 4:07
I’m okay, everything takes more effort and more time.
Bill Gasiamis 4:14
Everything takes more effort and more time. What happened to you, Alina?
Alina Gonzales 4:22
Mom, my mom will tell you more about what happened.
Barbara Gonzales 4:35
So we don’t both fit in the one chair. But my name is Barbara and I’m her mom. And she had a stroke close to two years ago. And it was unexpected. And she was driving and she felt very dizzy and she called 911 and they took her to the hospital.
Barbara Gonzales 5:00
And the emergency room attending doctor when I arrived a few minutes later told me that she wasn’t going to make it because the brain bleed was such that it was inoperable.
Barbara Gonzales 5:17
And she wasn’t responding, she wasn’t waking up. They’ve given her a sedative, and she’s very sensitive to medications. So she wasn’t coming out of the sedation. So a couple of hours later, she started to respond. And she was airlifted to another hospital where they tended to her needs and here she is.
Barbara Gonzales 5:43
She was in the hospital for about a month and a half and went to rehab as an inpatient for about a month and a half. And then came home probably about a year ago. And she’s trying to gain her mobility so she can gain her independence back.
Hemorrhagic Stroke Caused By an AVM – Alina Gonzales
Bill Gasiamis 6:09
Yeah. Wow. So what kind of stroke was it?
Barbara Gonzales 6:20
Hemorrhagic she was in a coma for about a month.
Bill Gasiamis 6:27
And do we know the cause of the stroke? Of the bleed?
Barbara Gonzales 6:32
It was an AVM.
Bill Gasiamis 6:38
Arteriovenous malformation. It’s what I had. And it seems to be very common in this podcast, but it’s a very rare thing. It’s only about one or 2% of the population that have AVMs.
Barbara Gonzales 6:52
It was too bad. She was very, obviously very health conscious. She had a great job with a pharmaceutical company. And she has her Master’s. She was an athlete in college, she had a scholarship and she played basketball for one of the schools here. And this was very unexpected. Has turned our lives in a different direction.
Bill Gasiamis 7:25
Yeah, yeah. That’s a pretty common thing for people to say about what stroke does to them. How old were you at the time Alina?
Alina Gonzales 7:36
40.
Bill Gasiamis 7:39
And there were no signs up until the day of the bleed. You had something going on in your head? Were there any signs whatsoever before that? Did you have a clue?
Alina Gonzales 7:49
No, I had no idea. It was a surprise.
Bill Gasiamis 8:02
Yeah, that’s a surprise, isn’t it? And since you got out of the hospital, what was it that you had to overcome? I realized that you have some speech challenges. Do you have aphasia? Is that one of the things?
Alina Gonzales 8:23
A little bit yeah.
Barbara Gonzales 8:24
Yes, she has a frozen rather not frozen, paralyzed vocal cord, her right vocal cord. And she was on a ventilator for about four weeks, I think and then she had a trach and she came home with a trach and she had it removed.
Barbara Gonzales 8:48
But her major problem right now is the dizziness and the lack of balance because she’s able to walk with assistance. But she can’t seem to stop getting those dizzy spells that are pretty constant.
Bill Gasiamis 9:07
And is always dizzy even when you’re sitting down?
Alina Gonzales 9:11
Yeah, it’s worse yeah. So the only time I don’t feel dizzy is when I’m lying down.
Bill Gasiamis 9:22
When you’re lying down is the only time you don’t feel dizzy? Does that mean that you’re lying down a lot?
Alina Gonzales 9:30
No, I’ve been working every day with my mom we go to the gym and walk the track about a quarter mile every day.
Bill Gasiamis 9:45
Yeah. And the dizziness, is it worse on some days and better on other days? Do you find a difference in sometimes the dizziness not being so bad?
Alina Gonzales 10:04
It’s bad every day.
Bill Gasiamis 10:10
Okay. So the sound of your voice, is that related to the tracheostomy that was used? Has that impacted your vocal cords? Is that what that’s done? Or is that impacted by the stroke? Do you know the difference? Do you know which one it might be?
Barbara Gonzales 10:30
They claim that it’s related to the stroke. My opinion having been by her side from the beginning, I feel that it was the trach that the trach was probably left in too long. And then when they did suctioning, the suctioning was done in a manner that, in my opinion, would cause some side effects. So we differ on that, on that opinion.
Bill Gasiamis 10:57
Yeah. Hard to know isn’t it? And it’s then also hard to I’m not sure about how you guys go about it, or how you feel about it. But whether or not you can lay blame or even whether it’s worth laying blame because what they’re trying to do is save Alina.
Bill Gasiamis 11:14
And it’s kind of one of the things that happened as a result of trying to save your life. So you kind of do you take the good with the bad? Does that annoy you that you also have to deal with that and that maybe somebody else was to blame for that?
Alina Gonzales 11:33
Yeah, I just want to be better. And communicate normally.
Bill Gasiamis 11:41
Yeah. Does your voice sound better than it used to Alina? Was it a lot more crackily than it is now?
Alina Gonzales 11:58
It’s better than it was.
Bill Gasiamis 12:02
It has improved?
Alina Gonzales 12:05
Yeah. For sure.
Bill Gasiamis 12:07
Excellent. What else has improved since the stroke?
Balancing Between Patience And Impatience While Living With Aphagia
Barbara Gonzales 12:16
Well I mean, cognitively she’s, she’s very good. So her walking has improved a great deal. And it’s been a slow journey with a lot more to do. And she’s impatient about getting it all done as soon as possible.
Bill Gasiamis 12:37
Well done. That’s pretty common. That’s well done. And also, be more patient, and well done for being impatient. Find the balance if you can, because by being impatient, you’re pushing, pushing, pushing for recovery, but that might frustrate you.
Bill Gasiamis 12:51
So if you get too frustrated, then you’re being too impatient. And then just like slow down a little bit. What I love about you, Alina is the first time we met you sent me a message on Instagram. I never knew who you were up until then.
Bill Gasiamis 13:07
And you said, Hi, Bill, I want to help. I’m 16 months post-stroke. How can I be useful? Thank you, Alina. I mean, I find that staggering and amazing and brilliant that you’re 16 months post-stroke, and you’ve got the challenges that you need to overcome, but you want to help other people.
Bill Gasiamis 13:33
Why do you want to help other people? And I love what you do. Don’t get me wrong. I’m not asking the question in that way to be silly. I’m just very curious as to what motivates you to want to help other people when you need plenty of help yourself.
Alina Gonzales 13:49
I think there’s a lack of understanding about stroke, I don’t think people understand what people go through when they have it and what it feels like to recover, I don’t think a lot of people understand, people need help and support.
Bill Gasiamis 14:18
Yeah, I love it. There’s a lack of understanding and what people are going through, through stroke. And other people out there who have had a stroke need to know that they’re not alone.
Bill Gasiamis 14:31
And we need to bring awareness to these situations. So what I’m seeing is that every time I interview a stroke survivor, that behind the I’m gonna call it the mask of stroke, behind the deficits behind the voice problems, behind the dizziness problems.
Bill Gasiamis 14:50
There is a “normal person” behind there who is still keen and interested in living a productive life. And is being interfered with by these things that stroke causes. Do you relate to that?
Alina Gonzales 15:07
Absolutely yeah, I feel like because I’m there, I show more. Because I know the life that I’m missing out on living.
Bill Gasiamis 15:30
You’re missing out on living? Yeah. And do you feel like in two or three or four years from now, you’ll be getting back to living your life again?
Alina Gonzales 15:50
I think so yeah.
Bill Gasiamis 15:52
Alright, you will. See that’s what’s important, what you just said is that I think I will be living my life again. And you will because I’ve met so many stroke survivors who have been through what you’re going through. And somehow, after 2 3 4, or 5 years, things do shift, and they start to find their way in the world.
Bill Gasiamis 16:15
And they start to become really important members of their community. I’m talking about the community that lives around them, their family, their friends, where they live, and go to the shops and do their shopping and all that kind of stuff, they start to become important they become creative, find creative ways to help.
Bill Gasiamis 16:40
And right now, I know this might not be what you want to hear. But it’s time to heal, time to rest time to do nothing, and time to do as little as possible. Other than putting all your focus and energy into just getting better and recovering. And it’s I know, it’s been 16 months, but it’s quite early in the stroke recovery phase.
Bill Gasiamis 17:08
You’re very, very early on. And I know you’re impatient. But if you could kind of get your head around the fact that it’s early, it’s not like a broken leg, then I think 2 3 4 5 years, there’ll be stuff that you’re still dealing with you have to overcome every day.
Hearing Loss Can Cause Balance Issues – Alina Gonzales
Bill Gasiamis 17:28
But things will start to shift in a direction that you’re controlling. And you’ll be back in control of your life. So the dizziness? What are the doctors saying about how to make that less of a problem? Do they have any ideas about how to support you with the dizziness?
Barbara Gonzales 18:02
Well, they’ve said that she should try and do vestibular training where she works through it without literally passing out. So generally, her impulse is to slow down when she gets dizzy.
Barbara Gonzales 18:22
What they’re suggesting is that she needs to head on and just keep pushing through it because the more she does that, the likelihood is that the dizziness will subside. So that’s the theory.
Barbara Gonzales 18:36
But she also had loss of hearing in her left ear. And she’s considering a cochlear implant because they’ve researched the fact that loss of hearing can cause a lot of imbalance. So we’re exploring that now.
Bill Gasiamis 18:56
Wow. So loss of hearing can also impact your balance.
Barbara Gonzales 19:06
Exactly, yes.
Bill Gasiamis 19:08
I’ve never heard that before. That’s got to be true. Because it makes sense, doesn’t it when you can’t hear out a year? It throws off your senses, and it might impact the way that you perceive the world.
Bill Gasiamis 19:25
And the way the brain receives information and then tells your body where it is in the world makes sense to me. So is the hearing completely gone in that year Alina?
Alina Gonzales 19:39
It’s completely gone.
Bill Gasiamis 19:46
Okay, so the cochlear implant will restore the hearing if you get that.
Alina Gonzales 19:53
Yeah.
Bill Gasiamis 19:56
Okay, so I interviewed one of the pioneers of the cochlear implant, also a neuroscientist Dr. Michael Merzenich, who is from the United States. And that’s going to be a very interesting episode for you to listen to. I think. Also, there are some people that you need to look into, and I’ll send you all the links.
Bill Gasiamis 20:28
And for the people that are watching, I’ll have links on the show notes, for the people that are listening as well. There’s a gentleman called Paul Becky reader. Back in the 80s, he used to work with people who had balance issues, and one particular lady was a lady who became unwell and lost her inner ear, her inner balance in the inner ear wherever that is.
Bill Gasiamis 20:53
And as a result, she couldn’t live her life. But then they rehabilitated her with this device that replaced Believe it or not that created with neuroplasticity, use the tongue to replace the inner ear balance mechanism. I can’t describe it well. But it was fascinating.
Bill Gasiamis 21:19
And there are videos of it on YouTube that you can watch. And there is also the interview with Dr. Michael Merzenich. And I’ll send that information. But also, for people who are listening and watching, you can go on to the recovery after stroke.com website, and click the podcast link. And there you will see the list of episodes.
Bill Gasiamis 21:45
And in that list, there’ll be a podcast that says we’ll find that right now. Rewiring The Brain, Michael Merzenich. It’s an amazing discussion on how far the study of neuroplasticity has come and how it’s helping people overcome some amazing challenges.
Bill Gasiamis 22:21
So what it does is offer hope but what’s also supported it’s a really big rabbit hole to dive down. And it’s also supported by a lot of research and studies so it’s legitimate and can improve lots of things for a lot of people.
Bill Gasiamis 22:40
I interviewed Dr. Merzenich, several years ago and the Episode Number is episode 108 for anyone listening and watching so you’re living at home with your mum now how has your life changed since the stroke? How were you getting about before the stroke?
Alina Gonzales 23:08
I can’t do anything for myself. So everything I need help with still, showering, going to the bathroom, cooking, I can’t drive I can’t walk, everything I need help with so I have no independence at all.
Bill Gasiamis 23:34
And before that what were you doing? How are you occupying your time?
Alina Gonzales 23:40
I was working, I had a really good job, and I was driving and I was doing theatre, I was in a local theatre.
Bill Gasiamis 24:00
Are you involved in the local theater? So you were an actor?
Alina Gonzales 24:14
Yeah.
Bill Gasiamis 24:15
Okay, so that’s a lot to lose, isn’t it?
Alina Gonzales 24:22
Yeah, I lost my job and the people I was with.
Bill Gasiamis 24:32
Yeah. Have you been able to reconnect with any of them recently?
Alina Gonzales 24:39
Yeah. I talked to them but it felt the same, I talked to them and they wanna know how I am.
Bill Gasiamis 24:59
Do you think it’s difficult for them to reconnect with you now that you’ve changed? And is it hard for them to know what to say do you think or how to behave?
Alina Gonzales 25:13
That’s probably part of it yeah. And they’re worried about not saying the right thing.
Bill Gasiamis 25:30
Is it possible for them to not say the right thing? Would you get offended if they say the wrong thing? Because they are ignorant, and they don’t know any better? Because they’ve never had what you’ve had? Would that offend you?
Alina Gonzales 25:43
No, not really. I understand because I already know that there’s a lack of understanding out there in general.
Bill Gasiamis 25:56
I love that. I mean, there’s no point getting offended is there? Because it’s not personal. It’s just literally people do not know what the hell is going on in the stroke world. And they don’t know how to respond or they don’t know how to speak.
Bill Gasiamis 26:09
And they don’t know how to make things better. And that’s what a lot of people try and do don’t they? They try and make things better. Because they want to help but they don’t know how to do that. So it becomes awkward.
Alina Gonzales 26:21
Yeah, that’s true. I want them to be honest, and upfront with me, but I think that they worry about things. Because I’m moving forward, I’m not stressed out about anything anymore, I don’t want to worry about things I worried about before.
Bill Gasiamis 27:04
What things were you worried about before that don’t matter anymore?
Alina Gonzales 27:12
Why do people like to stay away or at work, like why I wasn’t doing better at work? Or maybe somebody didn’t like me.
How Hard Is It For The Caregivers?

Bill Gasiamis 27:32
Why somebody didn’t like you? Why you weren’t performing enough? Why you didn’t do too well on that project? All the usual junk that in the end doesn’t make for a healthy or happy life, does it? At all, what’s it like for mum? Has Mum been able to share with you how difficult it is for her at the moment?
Barbara Gonzales 28:08
It’s difficult, but I’m so grateful to have her home. That’s the only thought that comes to mind when things get a little. A little dicey. I remember how it was when she was hospitalized and my only concern was getting her back to the house I’m so glad and grateful to have her here.
Bill Gasiamis 28:31
Do you still get cranky at each other Mum?
Barbara Gonzales 28:35
We have our days.
Bill Gasiamis 28:41
I mean, it’s normal, isn’t it? It’s normal to have somebody who’s sick and unwell, whom you want to do everything for, but then you also want to tell them off and tell them to shut up. Or do you want to tell them to be quiet or do you want to tell them to behave?
Barbara Gonzales 28:57
It’s more the other way around. But yes.
Bill Gasiamis 29:01
Alina mum, drives you nuts?
Alina Gonzales 29:05
No.
Bill Gasiamis 29:06
Are you honest? Are you being honest now?
Alina Gonzales 29:09
Yeah.
Bill Gasiamis 29:12
Look, we can all admit it a little bit. This is a bit like a therapy session. All right? So everyone can just tell the truth for a little bit if they want to. But if they don’t want to, it’s okay as well. We can all lie. There’s no problem at all.
Bill Gasiamis 29:24
I know how frustrating it was for my wife. She was caring for me at the beginning and man she copped so much abuse because I was not myself like I was in a completely different headspace in the world.
Bill Gasiamis 29:41
You know, like I was just gone. I was angry the medication was making me act up and misbehave and all sorts of things. And some of it was not only the medication, some of it was me as well. Right? Upset at what happened and all the usual stuff and I reflect on it now. And I know that she was doing a tough, I never knew how tough she was doing it.
Bill Gasiamis 30:04
Because she never told me because she was interested in maybe becoming well. And not making it about her. But at some point, I think caregivers need to make it about them, especially when it’s a 24-hour-a-day, seven-day-a-week job. Is that what is happening with your mum? Is it 24 hours a day, seven days a week that you’re with Alina?
Barbara Gonzales 30:31
Yes, it is.
Bill Gasiamis 30:33
And did you put your life on hold?
Barbara Gonzales 30:39
Oh, yes. There’s there’s nothing that goes on. That doesn’t revolve around her right now.
Bill Gasiamis 30:45
Yeah. And what was your life? Like, up until the stroke? What were you up to? How did you spend your days?
Barbara Gonzales 30:55
Well, I was I was babysitting with my two grandchildren. And then there were some illnesses in the family. And I thought that I just thought that, and then COVID This, this all happened. She got sick right around the time that COVID-19 started. So it’s just been it’s been like the world is turned upside down.
Bill Gasiamis 31:19
And is there anyone helping you out from time to time?
Barbara Gonzales 31:23
No, Not presently? No.
Bill Gasiamis 31:27
Right? And is there any support for somebody like you a caregiver and the person you’re caring for? Is there any way that you guys can access any support any kind of in-house support or external support?
Barbara Gonzales 31:41
I haven’t looked at anything right now. We’ve been so busy doing outpatient therapy. So we were driving a distance from home to get therapy for physical occupational and speech. So we’re, we’re really busy. So I know. We haven’t looked at anything like that.
Bill Gasiamis 32:05
It’s pretty common to be busy, at the very beginning of the whole stroke recovery, and working out how to solve all the little problems that turn up. And then at some point, when you start getting into a bit of a routine, and you have solved a lot of the problems.
Bill Gasiamis 32:24
Then maybe there’ll be some space or some time that’s created for you to start to get curious about what other support you can bring in how else you guys can support Elena, and also how you can give yourself a break because caregivers do it tough. And they need help and support as well. We need to make sure that the caregiver is healthy and well, there’s no point in having sick people.
Barbara Gonzales 32:52
That’s true. And I just want to say that we admire your work so much that of all of the people and all of the areas that we’ve looked into and researched. There is no single person that we enjoy hearing more than we enjoy hearing you. You’re just a wealth of information.
Bill Gasiamis 33:20
I enjoy you telling me that thank you so much. Yeah, I felt the same as you I was like Alina I wanted to share. I wanted to help because there was not enough known and when I went through my situation, it started 10 years ago, and I’m still going through it right now.
Bill Gasiamis 33:40
But clearly, I’m in a different situation than a lot of other stroke survivors, because we’re all different. I wanted to know how to help and what I could do, and I realized some people weren’t getting any support and weren’t getting any awareness about the situation.
Bill Gasiamis 33:59
Caregivers were one of those groups of people. And, then I felt like, if I’m going to interview people, I want stroke survivors to come on. But I didn’t know how bad stroke was because I got this version of it. And then I met people who can’t speak because of stroke who can’t see because of stroke, who speak but have got a different voice like Alina.
Bill Gasiamis 34:22
And then I had to make a decision. Because I used to be ignorant. I had to make a decision do I want everybody on my podcasts or just the people that can speak properly? And it’s like, how will I be able to share what stroke is really about if I just have people on that can talk like I can that wouldn’t be an accurate representation of stroke survivors.
Bill Gasiamis 34:48
So I’ve interviewed people that can talk like Alina, that have less ability to talk and some people that can’t talk at all, and we’ve used a machine recording to do that. So I also wanted to get caregivers on I wanted to get caregivers on because they are part of our community.
Bill Gasiamis 35:13
They are doing the heavy lifting as far as I’m concerned, and caring for people who need the support, but the caregivers don’t get any training. Mum, do you agree there’s no training, no support, no information about how you can do that well? And then also, at the same time, how to support yourself?
Intro 35:34
If you’ve had a stroke, and you’re in recovery, you’ll know what a scary and confusing time it can be, you’re likely to have a lot of questions going through your mind. How long will it take to recover? Will I recover? What things should I avoid in case I make matters worse?
Intro 35:51
Doctors will explain things that obviously, you’ve never had a stroke before, you probably don’t know what questions to ask. If this is you, you may be missing out on doing things that could help speed up your recovery. If you’re finding yourself in that situation, stop worrying, and head to recoveryafterstroke.com where you can download a guide that will help you.
Intro 36:14
It’s called seven questions to ask your doctor about your stroke. These seven questions are the ones Bill wished he’d asked when he was recovering from a stroke, they’ll not only help you better understand your condition, they’ll help you take a more active role in your recovery. Head to the website. Now, recoverafterstroke.com and download the guide. It’s free.
Barbara Gonzales 36:37
Absolutely none when she came home. We for some reason, because of COVID. We had no instructions on how to do anything. And she was on a feeding tube, which she still is, but I figured it out.
Barbara Gonzales 36:51
And it was very daunting to come home in a hospital bed with a trach and a feeding tube and not able to communicate I was told not to bring her home. They wanted her to go to a facility, a long-term facility and I didn’t want that. And I know that she’s thrived as a result of being here. She wouldn’t be as well as she is if she was elsewhere.
Bill Gasiamis 37:20
Yeah, I hear you. So you have to become a medical expert overnight, and nobody tells you how to do it. That is ridiculous. Doctors spend years and years in hospital to make sure that they don’t do the wrong thing. Are you concerned when you first come home that you might do the wrong thing and make things worse?
Barbara Gonzales 37:49
Oh, obviously, but it didn’t take me long to look, she’s on no medication. And it didn’t take me long to figure out that she was being overmedicated. And things that she was suffering from when she was in. She no longer had a problem with so I gained my confidence quickly.
Bill Gasiamis 38:10
So one of the people that you might love to listen to me interview guys is Duncan Campling. And he was on episode 133. And he spoke to me with a machine. So we did a little bit of preparation, and we wrote the questions down. We allowed him to record his answers on his voice, computer, or whatever it’s called.
Bill Gasiamis 38:40
And then we interviewed about a week later. So you might find that interesting. And everybody that’s been on the podcast just wants to share, they just want to help they just want to put stories out there. It’s a good way for families to kind of get an understanding of what is happening. So do you feel like this is something that is going to be worth sharing with the family? Are they going to be able to hear or watch this podcast episode?
Barbara Gonzales 39:14
Absolutely. Yes. It’d be great.
Bill Gasiamis 39:18
Yeah. Family and friends, because really, they’re the ones we want to know what’s going on. We also want them to know that we understand if they don’t know how to speak about what’s happened to us or how if they don’t know what to say it’s okay. If they say the wrong thing we won’t get offended might be a really good way to reach them without having to sit them down on one and have a conversation with them.
Barbara Gonzales 39:49
That’s true, that would be great.
Living with Aphagia

Bill Gasiamis 39:51
So Alina, are you still on a feeding tube because there’s a risk of choking when you chew and swallow food?
Alina Gonzales 40:02
Yeah if I swallow I could have aspiration. So my right vocal cord is still paralyzed. So I can’t swallow properly.
Barbara Gonzales 40:22
So, what she takes in because the right vocal cord isn’t working it could end up in her lung instead of her stomach. But she’s come a long way I mean she’s eating mashed foods now and we’re looking forward to having the tube removed once she can keep her intake at a level of the proper calories and the nutritional value.
Bill Gasiamis 40:56
Okay, so that’s improved as well. So you’re getting slowly able to increase what you have the kind of food that you eat, and then increase the amount that you ate so that you’re getting, say your regular 2000 calories a day or whatever the number is.
Bill Gasiamis 41:10
But at the moment, you’re not able to get that many calories through chewing it and through your mouth yet.
Alina Gonzales 41:17
Right.
Bill Gasiamis 41:19
Okay. So the tube is connected to where? Where is that attached? I know it’s somewhere around the belly. That’s your cat, hello kitty cat, the cat wanted to be on the podcast too.
Alina Gonzales 41:40
In my stomach.
Bill Gasiamis 41:43
It’s connected to your stomach. Okay. Aspiration is what happens when food goes into your windpipe instead of your throat.
Alina Gonzales 41:54
Yeah, instead of going to my stomach, it goes to the lungs.
Bill Gasiamis 42:00
Yeah. Okay. So you’ve found over time that that’s getting better? And is there some kind of a goal or some kind of a timeframe where you’re hoping to move from being tube-fed to being fully able to eat normally, or something close to normal?
Barbara Gonzales 42:25
Her speech therapist thinks that maybe in a couple of months that might be possible. So she’s off, when she came home, she was on continuous speed, which really limited movement for her and all but I figured out how to give her the bolus feedings. And, so she’s eating, she’s happy that about three times a day, which is great, because that way she can get around without being attached to anything.
Bill Gasiamis 42:54
Right, right. So mum you’re gone back to caring for the child that you already cared for when she was born. Are there similarities? Is it a completely different experience? How do you relate to this version compared to the first time?
Barbara Gonzales 43:20
Do you know it’s indescribable, number one, but I can only tell you that I do see light at the end of the tunnel here? And I know that she can improve. And I know that this isn’t a permanent situation. So it’s just getting through it. That is the journey. So I’m hopeful.
Bill Gasiamis 43:44
Do you agree Alina?
Alina Gonzales 43:51
Yeah, I have to get better.
Bill Gasiamis 43:53
Yeah, you have to do and you will, things will improve. Is she a pretty cool mum?
Alina Gonzales 44:02
Yeah, I feel very lucky, at the end of the day I know how lucky I am.
Bill Gasiamis 44:14
Yeah. She’s a pretty cool lady. I can hear that in her voice, I love the psychology that she used to approach this situation, you know, it’s a situation where things are difficult, but they’re going to get better. We have to get through it. It’s indescribable. But we have things that we need to achieve and overcome and it’s not permanent.
Bill Gasiamis 44:46
And I love that that is probably one of the best things that I’ve heard on a podcast is that this particular current state in situation although it feels quite possibly, you know, being shiny an ongoing and never-ending, it is not permanent, you will shift and change. That’s a great way to think about things.
Alina Gonzales 45:10
Recovery is so slow, that’s the thing I was unaware of before.
Bill Gasiamis 45:22
Yeah. It is so slow. I would love to have you guys back on the podcast 12 months from now to show me how far you’ve come.
Barbara Gonzales 45:33
That would be great.
Bill Gasiamis 45:37
All right now, Mum has remained behind the camera for this whole time. And she hasn’t revealed herself. We don’t even know her name. So why don’t we get Mum in front of the camera? And we can get to see her and we can ask her name.
Barbara Gonzales 45:56
There you go.
Bill Gasiamis 45:57
That’s not enough. That’s not enough. Hey, hello.
Barbara Gonzales 46:04
My name is Barbara.
Bill Gasiamis 46:05
Hey, Barbara. Lovely to meet you.
Barbara Gonzales 46:08
And I’m so thrilled. You are just really special to us your voice. Whenever I hear your voice. I come running to hear what it is you’re saying.
Bill Gasiamis 46:17
Thanks so much, Barbara. How old are you? You look so young.
Barbara Gonzales 46:22
I’m so old.
Bill Gasiamis 46:24
You don’t look it, how old are you?
Barbara Gonzales 46:28
This is a podcast other people will be hearing this I’d rather not. I turned 66.
Bill Gasiamis 46:36
Okay. Well, you look so young. You look fit healthy, and energetic. That’s where I was getting at. You guys look like, there’s not a lot of gap between you in age. And yeah, I was kind of right. It’s only 26 years. It’s nothing. You’re a young mum?
Barbara Gonzales 46:53
Yes. Yes. Very young.
Bill Gasiamis 46:56
Yeah. Well, I can relate to that. I was a young dad, I was 22 when I became a dad.
Barbara Gonzales 47:02
That sounds about right. Yeah. That is too young to have children.
Bill Gasiamis 47:08
Too young to know what the hell you’re doing let alone raise kids right?
Barbara Gonzales 47:14
And your children are how old now?
Bill Gasiamis 47:16
25 and 21.
Barbara Gonzales 47:20
Wow, that’s incredible. Right? He looks so young himself.
Bill Gasiamis 47:24
So that’s the thing. I’m trying to get my head around the whole age gap. And I think it’s great to be young and energetic when you have kids because you guys can support each other for a long, long time to come. And that’s kind of one of the benefits that I didn’t realize that I was going to be able to have when my kids were so young.
Bill Gasiamis 47:49
And I was so young when I had the stroke, I was 37. So they that that lack of old age, between, you know, that lack of gap between me and my kids meant that they kept me young and I had something to focus on and something to aim towards getting better about and something to teach them and to leave them better for what happened to me like to kind of give them life experience without going through the tough hard parts of it. Does that make sense?
Continuous Learning

Barbara Gonzales 48:23
You have such a great attitude, you do such a solid, so centered, and truly balanced. I enjoy hearing you.
Bill Gasiamis 48:33
Yeah, I try to it’s something that I work on. And you know, people who listened to me sometimes. And I asked him to be in a podcast, I get all flustered, you know, what am I going to say it’s Bill, Bill wants me on the podcast. And it’s like, I’m just a regular guy learning all the same stuff that you’re learning, and I don’t know how well I’m doing until I’ve become better.
Bill Gasiamis 48:56
And I reflect on how far I’ve come. So I’m constantly in this learning phase like you guys about, you know, what’s the best way to go about this. We can choose a way that’s difficult and mentally challenging. And we can suffer through that. But that’s not the most useful we suffer regardless of which way we go forward, we may as well use suffering to our advantage to get something out of it.
Bill Gasiamis 49:27
And that’s kind of what I see you doing. You said it you know this is only temporary in this current situation. And I love what you said it’s about what’s going to happen in the next and how things will change for the better in the next two, three four five months six months, or a year.
Bill Gasiamis 49:44
So I just hope that my thinking is making other people think and if they disagree with me, I’d love to hear from them. Tell me you know, come on board to the podcast, leave a message On YouTube or, you know, give me a thumbs up or thumbs down, I don’t mind.
Bill Gasiamis 50:05
But I think this is the only way we’re gonna get through it together, right? And it doesn’t matter how far we are in the world. We can all help and support each other. And you think that I’m helping you and I am. But you guys are also helping me. That’s what’s important for the people who come on this podcast to also know.
Barbara Gonzales 50:29
It’s amazing how an experience like this also makes you realize how much you can do that you didn’t think you were able to do. That’s always an eye-opener.
Bill Gasiamis 50:41
That is such an eye-opener. Look, it’s such a pleasure to see you both. Thank you so much for being on the podcast. Alina, I’m going to invite you back in a year. Right? We’re going to do this again. So is there anything you want to say to leave us with before the end of the episode?
Alina Gonzales 51:00
Just don’t give up.
Bill Gasiamis 51:09
Don’t give up. I couldn’t agree more. Thanks so much for being on the podcast.
Alina Gonzales 51:13
Thank you so much.
Bill Gasiamis 51:17
Well, thanks for joining us on today’s episode. I hope you’ve enjoyed that conversation and got something out of Alina and Barbara’s story. They’re both amazing ladies and support each other to get through this. And I think that what I have to share should make and will make a huge difference for a lot of people.
Bill Gasiamis 51:39
Please comment, like, or share. Wherever you see this podcast episode. If it’s on YouTube, give us a thumbs up, leave a comment, like, share. If it’s on Instagram, and you’re just seeing a small amount of this share let me know what you think give me some feedback, every interaction will make a big difference to how the show ranks on social media.
Bill Gasiamis 52:01
As a result of that, it will make it easier for other stroke survivors to find the show and hopefully, it’ll support them to have a better stroke recovery. So thanks for listening and see you on the next episode.
Intro 52:14
Importantly, we present many podcasts designed to give you an insight and understanding into the experiences of other individuals’ opinions and treatment protocols discussed during any podcast or the individual’s own experience and we do not necessarily share the same opinion nor do we recommend any treatment protocol discussed.
Intro 52:31
All content on this website at any linked blog, podcast, or video material controlled by this website or content is created and produced for informational purposes only and is largely based on the personal experience of Bill Gasiamis, the content is intended to complement your medical treatment and support healing. It is not intended to be a substitute for professional medical advice and should not be relied on as health advice.
Intro 52:31
The information is general and may not be suitable for your personal injuries, circumstances or health objectives did not use our content as a standalone resource to diagnose, treat, cure, or prevent any disease for therapeutic purposes or as a substitute for the advice of a health professional.
Intro 52:31
Never delay seeking advice or disregard the advice of a medical professional your doctor or your rehabilitation program based on our content if you have any questions or concerns about your health or medical condition, please seek guidance from a doctor or other medical professional if you are experiencing a health emergency or think you might be, call triple zero if in Australia or your local emergency number immediately for emergency assistance or go to the nearest hospital emergency department.
Intro 52:31
Medical information changes constantly. While we aim to provide current quality information in our content. We did not provide any guarantees and assume no legal liability or responsibility for the accuracy, currency, or completeness of the content. If you choose to rely on any information within our content, you do so solely at your own risk. We are careful with the links we provide however third-party links from our website are followed at your own risk and we are not responsible for any information you find there.






