Saran Chamberlain was 37 when she experienced a right ischemic stroke, caused by a carotid artery dissection
Socials:
Highlights:
01:09 Introduction – Saran Chamberlain
04:01 Carotid Artery Dissection Recovery
09:18 Parenting During Recovery
13:13 Dealing With Emotions
19:59 Reflection In Recovery
24:56 Celebrate The Small Wins
34:58 Reaching Out To Other Stroke Survivors
43:41 Saran Chamberlain’s Identity
51:15 Someone On The Inside
57:37 All About Stroke
Transcription
Saran 0:01
So how was it navigating the children when you first got home and then all of that stuff, I know you keenly probably wanted to get back to the children and be at home and resume your duties as normal. But it wasn’t normal. When you get back. What was that like?
Saran 0:20
It wasn’t. And the emotion and the, the fact that basically, there’s no filter was just so hard. And so my youngest, who’s now 12, I used to come in and she used to want to, you know, play with me and I would say I’m just exhausted, I cannot do it, and I would cry, and she would get so upset. And luckily my mother-in-law lived with us at the time. And so she would sort of help her through.
Intro 0:55
This is the recovery after stroke podcast, with Bill Gasiamis, helping you navigate recovery after a stroke.
Introduction – Saran Chamberlain

Saran 1:09
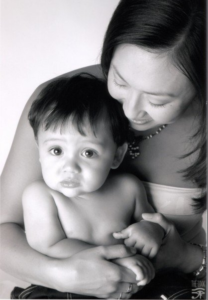
Hello, and welcome to the Recovery after Stroke podcast. This is episode 183. And my guest today is Saran Chamberlain, who was a young mum with three children aged three, seven, and nine. When at age 38, she experienced a right ischemic carotid artery dissection.
Bill Gasiamis 1:29
Now nine years on, she has overcome a lot to go back to work and is heavily involved in the organization she founded called Young Enabled Stroke Survivors, South Australia, an organization that assists and empowers young stroke survivors aged 65 and under to live their lives to the best of their ability. Saran Chamberlain, welcome to the podcast.
Saran 1:54
Thank you for having me.
Saran 1:56
Thanks for being here. Appreciate it. It’s good to have a fellow Aussie on the podcast, it’s very rare actually, I think the majority of the people I interviewed tend to be in the United States. And Australia is a very, very distant second.
Saran 2:20
Well hopefully, we’re finally more, as we’re going along in social media.
Saran 2:26
Yeah, more people to help and support and who need your help and we need to make up communities. Tell me a little bit about what happened to you.
Saran 2:33
So nine years ago, I was 38. And I was fit and healthy. I have three kids that were three, seven, and nine at the time. And I didn’t have anything that sort of gave any warning. But in the morning, I went to tidy up my daughter’s bedroom. And I lost feeling in my left arm. And when I stood up, I couldn’t feel my left leg.
Saran 3:00
So yeah, it’s a bit of a shock. That was it. I was awake the whole time. I can remember everything. Luckily, my partner recognized that it was a stroke. So I was in hospital within about 15 minutes. They thought it was a migraine for probably a good 24 hours even though they tried the thrombolysis.
Saran 3:23
And it wasn’t until at the time there wasn’t a 24/7 stroke unit, but there is now in Adelaide. And yeah, I had a couple of CAT scans. And then by the time I had the MRI, they worked out that it was a clot. It was a right ischemic stroke.
Saran 3:42
So carotid artery dissection went into the sensory premotor and motor cortex of my hand and fingers, so I had to learn how to walk again. I had nothing in my hand for quite some time. Yeah, it’s been a bit of a journey.
Carotid Artery Dissection Recovery

Saran 4:01
Especially with the little kids, my gosh. Going through the stroke and trying to raise the children. So how long were you out of action in the initial phases from that day that you noticed the numbness? How long were you out of action?
Saran 4:19
So I was severely stubborn from the very start. I’m thankful that I still had my general stubbornness and wits about me. They told me I’d be in hospital for about a month and rehab for three months. I was in the hospital for eight days and rehab for three weeks as an inpatient.
Saran 4:42
They couldn’t keep me in for much longer than that. But I suppose it took me probably a good three months to be able to walk without a stick. But my therapist from the very start was strict with me so I was banned from living outside of my bedroom when I first got to rehab.
Saran 5:00
So I got told off a lot because you know, she was sort of saying, You need quality movement. So she got rid of my quadstick and gave me a stick. And yeah. So gave me sort of limits. And I kept sort of breaking those. But yeah, so I was home after about a month but still doing rehab every day.
Saran 5:26
I got my license back in three months so that was good. I drive with a steering knob. And so I can still get myself out. But obviously, the biggest thing has been fatigue, sensory overload, and all the fun stuff that people just don’t see.
Saran 5:47
Is that still now? Or was that at the beginning when you first went home?
Saran 5:52
Yeah. So I remember going to a pain specialist probably about a year and a half afterward and saying, so this fatigue, you know, when am I getting rid of it? And he said, No, you have fatigue and I said, yeah, I know, but when am I getting rid of it? And he said, No, no, you have fatigue, and you will have it for the rest of your life.
Saran 6:10
And you just need to learn to deal with it. And he wasn’t a very good pain specialist. But he told me the truth in that respect. I think I’ve worked out now that one, my body always wins. And I just go with it. And I know that if I’m learning something new, or if I have meetings, then I know that that sort of takes it out of me a little bit more.
Saran 6:38
But generally, now I think I’ve got it fairly under control as to, you know, I still have rests during the day, probably every second day, at least. And that’s just, you know, that I set my alarm for 45 minutes, and just let myself stop and let my body rest. And I always wake up and kind of go, thinking of a break and getting a rest but the body’s fine. So then so is my head, so it’s good.
Saran 7:10
Yeah, I kind of have to do an automatic 45-minute or an hour kind of power rest. These days, it’s not sleeping or anything like that.
Saran 7:25
Yeah, you’re still sort of conscious and can hear everything. It’s just stop, isn’t it?
Saran 7:30
Yeah. So it’s like a reset, like laying down reset, getting everything kind of, okay again, and then getting up and going, Okay, I feel better, I can get on to the following tasks, new tasks, require a lot of concentration fatigue may still kind of frazzled me a little bit, but the majority of the fatigue has gone away in that I’ve found the limits and push them and push them and push them.
Bill Gasiamis 8:01
And now I know, there’s no more pushing them. They’re just, they’re just further down the day than they were, they used to be early. And for a long time, that’s kind of stretched out the amount of hours that I can go before the body says enough. And if I’ve had good sleep for several days in a row, then it’s even better, but I find that the lack of sleep will determine how much fatigue I’m gonna have to deal with. On any given day.
Saran 8:34
I’ve kind of worked out that it’s like this little friend that just comes along with you for the trip. And you’re never going to get rid of it. So you just have to kind of you know, it’s this to get along. And if you don’t get along with it, you know, there’s a problem because you never gonna separate. So yeah, it’s just kind of like, okay, this is what you want to do. Fair enough.
Saran 8:59
So how was it navigating the children when you first got home, and then all of that stuff? Because I know you keenly probably wanted to get back to the children and be at home and resume your duties as normal. But it wasn’t normal. When you get back. What was that? Like?
Parenting During Recovery
Saran 9:18
It wasn’t, and the emotion and the fact that basically, there’s no filter was just so hard. And I still so my youngest, who’s now 12. I know I used to come in and she used to want to play with me and I would say I’m just I’m exhausted, I cannot do it. And I would cry. And she would get so upset.
Saran 9:44
And luckily my mother-in-law lived with us at the time. And so she would sort of help her through. We ended up sort of working out that the best way for us to play was after when I sleep and then she’d come in, I’d be sitting in my bed and she’d sort of play shops with me.
Saran 10:03
So as opposed to perhaps, you know, before where I would go out, and you know, to hang out with them, she would come in with me. I was able to at least still take them to school. I stopped cooking, although I never really cooked before. But, yeah, again, the kids had to just learn that there were times when, like, in the afternoon, they had to be quiet.
Saran 10:32
And they had to learn to basically, look after me, which was hard, you know, to sort of change things around, turn those tables. And I did worry that you know, the kids are gonna grow up saying, I didn’t have a family, you know, I didn’t have a childhood, because I had to look after my Mum.
Saran 10:52
But they are so empathetic. And so understanding and so I sort of say that they weren’t in that childhood, selfish bubble, they’re always aware of things. And I, you know, I say that our journey was a family journey because we were that close. And we had to do it all together to keep going.
Saran 11:17
I had teenagers at the time, and I like to think that they’re even worse than young children who actually, don’t get it. Because teenagers, I think choosing to not get it was frustrating coming home, because I’d come home between sort of 4:00 and 4:30 in the afternoon, and my job would be to prepare dinner and all that kind of stuff because my wife would be home at 6:30.
Bill Gasiamis 11:44
And the kids just wouldn’t play along to the I need your help. Pick this up, do that, you know, prepare dinner prepare the table, whatever, they just wouldn’t come along for the ride, they were teenagers, they were totally and utterly selfish, couldn’t care less about what I was going through, they’re boys. So it’s even harder to sort of try and bring them along, for the domestic side of it.
Bill Gasiamis 12:14
And maybe they also were never really taught to be domesticated by us early on, we didn’t kind of see a need for them to be involved at that level, they did help out from time to time with certain chores, but nothing major. So retraining them was impossible.
Bill Gasiamis 12:32
The bad habits were well and truly established by the time I needed to get them to come over to my site, and I would just freak out, I would lose it, I would yell and scream at them, all at the same time, when I’m trying to be better and nicer, and all those types of things.
Bill Gasiamis 12:47
But the frustration, the challenges of the fatigue, and the fact that I couldn’t do it alone, there was no way that I could do it alone just made me lose it and scream at them and get them to sort of shock them into doing something for me. And then I find myself, you know, hating myself and apologizing and feeling terrible, but it was such a vicious cycle.
Saran Chamberlain Dealing With Emotions
Saran 13:13
So have you spoken to them since like and as to like, their understanding and memory of that time? Because that’s sort of what I did is, you know, do you remember, I mean, my kids now sort of go remember the stroke. And this is just sort of what we do now. And probably I was lucky that they were young. Yeah, but like do you remember, sort of fighting that at all?
Saran 13:44
I think they might have rolled it into my old, cranky shitty self, you know, and kind of thought this is just another level of it. Because I was, I was a good dad, I was a good guy, all that stuff, good husband, but I was so under-resourced in my life like I didn’t have resources to know how to manage different emotions and different frustrations.
Bill Gasiamis 14:06
And I was pretty stupid. Like I was pretty thick, unintelligent, in that way. Very much lacked emotional intelligence. And I feel like my wife was on a similar level as me. You know, we weren’t skilled at communicating our needs. And we were helping we help each other the way that we thought other people needed help rather than the way that they needed help.
Bill Gasiamis 14:33
So the kids kind of just got well this is just him being normal again, but a lot of what they were getting that was extra was that we’re getting the apologies which I never really knew how to do before or understood that I needed to do or so that we get a lot of apologies to say look, sorry for before and all that type of thing, and I will try to explain to them what my frustrations and challenges were We’re, but they didn’t get it.
Bill Gasiamis 15:02
And it’s, I understand that they didn’t get it. Because the other level of it is, how can you possibly understand what somebody is going through unless you’ve been through it? And you never want them to go through what we’ve been through for them to understand you totally and utterly.
Bill Gasiamis 15:18
So yeah, it was just one of the hardest things for me. And now that they’re older and they’re in their 20s. Our interactions are very different, you know, still, we play the parents and child kind of role, but we’re evolving into adult and adult roles, you know, and it’s taken ages, but there was no other way to go about it. That’s the only way.
Saran 15:52
I feel like, I mean, you know, I was working stupid hours and traveling so much. And I think that if it wasn’t for the stroke, you know, there’s lots of reflection, of course, after stroke after a trauma. I know, that I wouldn’t have had the relationship that I do with my kids now had the stroke not happened.
Saran 16:13
And so, while you know, they’re still kids and tease me and do their usual stuff we are such a close unit that yeah, I sometimes, you know, I mean, I came home the other day, from Melbourne, and I had some more feeling in my arm, and they’re also excited for me, and yet, they’re all still, you know, teasing me and being idiots. But, you know, stuff like that would not have happened pre-stroke at all. And I know that, and I’m grateful for stuff like that.
Saran 16:53
Yeah. Too serious, too busy, too stressed, too focused too whatever.
Saran 17:00
Yeah, yeah, there was no time in my life for my kids. They were, I would pass them, you know, I would work stupid hours. And even when we went on holiday, once my partner and I, David, wrote diaries. And so you know, it says, David’s written, I called our family, and Saran called her family, which is work, you know, and it was just, it just was. And yeah, I look at it now, I think, Wow, imagine, you know, like, I still sort of go, what would have been like, now, you know.
Saran 17:41
We would just be crude, stupid, just, you know, you’re learning, you’re still evolving, you’re still trying to get a sense of growth and wisdom out alive. And it just takes ages to get there.
Bill Gasiamis 17:55
And you kind of have to fumble your way through stroke with the resources you’ve managed to build up in your life. And, doesn’t matter what you’ve got built up, there are not enough resources to deal with stroke, you have to learn new ones the hard way, there’s no other way, right?
Bill Gasiamis 18:12
So I considered myself stupid. And for the stupid people out there, don’t worry about it. Like you’re going to evolve, you’re going to get better, you’re going to grow. And you’re going to learn new skills. And you’re going to look back and go, man, God, I was sick. But I’m better now. And I’ve taken the lessons and it’s enhanced my life in these ways. Does that make sense? Do you relate to that?
Saran 18:40
Yeah, absolutely. I mean, I think we’re pretty hard on ourselves. So I’m sure other people I’m sure, I’m sort of thinking I’m sure you weren’t stupid. I just think we just learned to cope with what was being thrown at us, which is usually a hell of a lot. And so you don’t have time to consider and try and, you know, think about, well, how other people might be better how our kids might better respond to things.
Saran 19:07
You know, we only do that afterward. Because basically, one we have a hell of a lot of time. But also, we’re suddenly learning all over again, how to actually, you know, deal with our own lives, let alone everyone else’s that’s connected with us.
Saran 19:22
And you have new levels of challenges that you need to and problems that you need to solve that you’ve never had to solve before. So the old way doesn’t work for me. The old way did not work. If I continue to go down that path. It would just end in disaster.
Bill Gasiamis 19:39
So it was like, okay, you’ve got to find a new way and the new way was better and then I was able to reflect and go, Oh my God, if I was doing that earlier, that would have been so much better, but I wasn’t. I’ll start doing it now, and yeah, things kind of improved, and my level of intelligence at every level kind of improved.
Reflection In Recovery
Bill Gasiamis 19:59
When I realized that the old technique of managing my household and my relationships and my children and all that kind of stuff was just not going to work. There was just no way. So it was up to me to step up and deal with stroke, evolve, and learn and discover new ways.
Saran 20:25
It’s Yeah, it’s amazing the reflections and things that we learned like again, I think that you know in some ways, it’s really difficult that we can still see our life pre-stroke, because we’re comparing, you know, we’re comparing that, but then if we just look at, you know, what we’ve done post-stroke, and how we have actually sort of evolved and how we have ridden the wave.
Saran 20:57
Again, if we look at it, you know at each other from our, you know, from each other’s perspective, you know, we realize how far that person has come. And I think sometimes we need to give ourselves a bit more credit for that. Because again, we’re still like, we still could be doing better. You know, but that’s, I suppose that’s life as well, isn’t it?
Saran 21:19
Yeah. And I think reflection is really important in recovery because you can focus on the wins, rather than on all the negatives. After all, there’s so many in stroke recovery, there’s, you know, there could be more negatives than positives if you spent enough time on it.
Bill Gasiamis 21:35
But the reality is, the positives are what sort of fill your wings and lift you a bit further and keep you going. And, and that offers more hope. And then with hope, changes perspective and focus and all that kind of stuff. And you go after things that you may have been told were not possible way back whenever and, that kind of gets you to the other side.
Bill Gasiamis 21:59
I didn’t focus on the negatives, and I haven’t, in life, I tended to get caught up with things like if I didn’t know the path forward, I might never take any steps toward the destination. So for example, when I was early, in my years, I wanted to in my 20s, I wanted to start my own business and work for myself, but I didn’t know what the first step was.
Bill Gasiamis 22:32
So then, it seemed like procrastination. But I never did anything for eight years until someone taught me or I learned somewhere what the first step was. And then I made the first step. And then the other steps revealed themselves. So that was, that’s kind of it and I never focused on the negatives, I just focused on what I didn’t know, I don’t know these things, therefore, I’m not doing anything.
Bill Gasiamis 23:01
Whereas in stroke recovery, I know some people focus on, well, my leg doesn’t work, my arm doesn’t work, or this doesn’t work. And then they get stuck there. Whereas I was always focusing on Okay, well, the left side of my body is not working well, I’ll just drag myself with the right side, you know.
Bill Gasiamis 23:17
Or you were kind of always looking for the solution to the challenge at the time. And that was what moved me forward. And I’m always a half-glass half half-full kind of guy. So I, I hear when people say they focused, you know, they got sort of stuck in cycles of negativity and all that kind of stuff. I just don’t know how they did it, because I didn’t do it. But I can understand why they did it.
Saran 23:44
Yeah. I mean, I had some tough times and what I did learn was just like, with, I suppose the whole journey was, you know, early on, I fought it because I think no, I don’t want to feel bad. Like, you know, I’m not feeling this way. I’m just gonna put it away. And of course, all it did was exhaust me. But also, it was still there.
Saran 24:08
Once I’d worked out that, okay, I’m gonna go with this and I’m going to feel like crap when I feel it. And I knew that I was going to come out of it sort of the other side with it looking brighter with me with more energy because I hadn’t fought it.
Saran 24:25
And then I can actually go right, right, dealt with that now you can sit back there, and I’m still aiming for so I found that once I did that, and it probably took a couple of years, few years four years and but yeah, I do that I think I sort of doing that with most things now. The good and the bad. Just going with it, but yeah, still make sure that I celebrate the small wins because you know that’s what keeps you moving.
Celebrate The Small Wins – Saran Chamberlain

Saran 24:57
Yeah, and they all add up into a big meaning you just can’t see it yet it hasn’t yet happened. So you know those little wins 1 2 3. And then however many there are, by the time you get to that big win, where you can look back and go, Oh, my gosh, this is how far I’ve come? Wow, I didn’t realize it was all those little steps.
Bill Gasiamis 25:16
And it’s, for me it was a bit counterintuitive is not focused on the massive goal, which was, for example, walking, it was just focused on the little goals, that I kind of knew were part of the massive goal somewhere down the track. And then I would eventually get there, and therefore that would be fine.
Bill Gasiamis 25:35
The other thing I found was that timelines and deadlines on when things would happen weren’t going to be useful. So what was that like for you? Did you kind of have these expectations of when you’d be reaching certain milestones?
Saran 25:49
That one-year mark? Hell, because you’ve got to the one year and kind of went, wait, I’m not done. Shit, I go hang on a minute, what? Like, you know, and I remember, I remember, it’s probably the one time I rang Stroke Foundation, I spoke with Simone she was amazing.
Saran 26:10
And basically, I said, you know, I was able to walk fairly quickly, my arms there’s nothing to my arm, but I can still move around. But I thought I’d be better by now. And, yeah, I’ve learned it’s a journey. And as long as I’m still moving forward, then I’ll just keep going, I don’t set timelines anymore. I don’t set recovery goals, you know, I set you know, I hope to be able to walk further.
Saran 26:42
You know, not I’m going to walk, I don’t know, five K’s without falling over. I want to have less foot drop, I want to be able to, you know, do those kinds of things to set recovery goals means that you know, you’re going to get to an end goal. And, you know, and that Yeah, I think that takes a little bit of time, doesn’t it?
Saran 27:05
Because I think we always have seen, you know, we’ve always looked at goals. But when it comes to stroke, because it’s your life, it’s you know, it’s not going to ever be better, even if everything, even my hand sort of got better. I don’t think you know, fatigue and sensory overload wouldn’t be gone. So it still, you know, it’s there. It’s just how to deal with things you deal with in your life. easier, better.
Saran 27:36
Yeah. Goals. For me, like I said, they were kind of big, but at a distance, they weren’t really about me achieving them right now. And they just took the pressure off, I think, and therefore, if I didn’t put a timeline on it, or also took the pressure off, it was about getting good at what I was doing then, rather than focusing on what the big far distant end goal was going to be.
Bill Gasiamis 28:04
So I can relate to that. I know, a few people that I’ve supported and coached through stroke recovery, you know, will tell me, but it’s been 12 months, and I should be better by now. I’m like, where did you get that information from? You know, who gave you that 12 months is early on in your recovery?
Bill Gasiamis 28:22
It’s early days, you know, it’s probably just like, if, if a broken toe is the day you broke it is when the beginning of 12 months is pretty much the day you had the stroke, it’s the first moment you still need time to get beyond that. And it’s different from a broken toe. It doesn’t have a doctor’s you know, six weeks, three weeks, you come back and you take this off for weeks, we check it, five weeks we do that and what six weeks you’re back at wherever you were doing whatever you’re doing.
Bill Gasiamis 28:58
It just doesn’t have that. And I know if you can get people to stop focusing on the timeline and anniversary and all that kind of stuff, then it gets better. Speaking of anniversaries Did you ever focus on Did you ever get to your anniversaries and be concerned about?
Bill Gasiamis 29:19
I don’t know having another stroke. I hear some people who have had a terrible time on the first and second anniversary. It either brings back the trauma or it makes them think that they’re about to have another one or they’re worried that they might have one.
Saran 29:36
No, mainly because our family is fairly good humor out on my anniversary and my kids and David used to go to the hospital, although it’s now been demolished as a new one. And then they tried to do that with the rehab hospital and then that got that was replaced anyway, but that would go to the room. Each year and sort of say, oh, you know, my mum had a stroke X amount of years ago, she’s okay.
Saran 30:04
Because they’d have to make sure that initially, it was like Lily, she’s fine. But we come here to celebrate that, you know, this place he’ll do and that kind of thing. So it was a bit of a celebration.
Saran 30:16
I was told that there was no real cause of my stroke and that, and that was a good thing because it probably wouldn’t happen again. So I had no pre-existing conditions or anything like that. So I didn’t really have too much of a fear around that time, or at all, maybe if I had a bit of a headache, but again, I didn’t even have a headache when I had the stroke. So yeah.
Saran 30:40
Yeah, just one of those things.
Saran 30:43
One of those things.
Saran 30:44
That’s interesting. So you’re pretty active in the community. In South Australia, specifically, the organization that you’re a part of is the Young Enabled Stroke Survivors of South Australia essay. And you’re involved with a couple of other people who are pretty awesome.
Bill Gasiamis 31:07
Peter Dempsey is somebody who I interviewed way back in episode 33. And Peter was talking about recovery from aphasia and childhood stroke. So I think when I interviewed him, he was, well it wasn’t that long ago. So you know, he’s an older bloke, but not that old. But he had a stroke when he was a young child. Tell me a little bit about it, Yes SA.
Intro 31:38
If you’ve had a stroke, and you’re in recovery, you will know what a scary and confusing time it can be, you’re likely to have a lot of questions going through your mind. Like, how long will it take to recover? Will I recover? What things should I avoid? In case I make matters worse, doctors will explain things that, you’ve never had a stroke before, and you probably don’t know what questions to ask.
Intro 32:03
If this is you, you may be missing out on doing things that could help speed up your recovery. If you’re finding yourself in that situation, stop worrying, and head to recovery after stroke.com where you can download a guide that will help you it’s called Seven Questions to Ask Your Doctor about your Stroke.
Intro 32:22
These seven questions are the ones Bill wished he’d asked when he was recovering from a stroke, they’ll not only help you better understand your condition, but they’ll also help you take a more active role in your recovery, head to the website now, recoveryafterstroke.com and download the guide. It’s free.
Saran 32:42
So it started with Susan Hillier, and I, just because we were talking about the fact that, you know, I wanted to get back to the gym, get back to Pilates and that kind of thing. And that, you know, I was never going to put myself in a position where, you know, I would walk in and people do anyone have any injuries, and you know, you put your hand up.
Saran 33:06
And so I’ll say I had a stroke, and they’re like, oh my god, I’m so sorry. And, you know, and it’s bad enough that people will stare at you anyway, let alone in a room that you’re then in with them for the next hour. And so we wanted to sort of look at, you know, arming people who had brain injuries, with the, you know, with the confidence to be able to go into any class and to know things that they were and weren’t able to do.
Saran 33:18
So I met Peter at one of the stroke forums and his right arm doesn’t work, so it’s kind of funny when we sort of hug each other because kind of an awkward, you know, lopsided kind of hug. And, okay, of course, because his stroke was on the other side, his was aphasia, mine was physical. So we sort of said, Hey, let’s, you know, let’s team up because we’re, you know, sort of one person ideally, or, you know, one stroke, put together kind of thing.
Saran 34:05
And, yeah, and so, South Australia is quite small compared to Melbourne, Sydney, you know, we wanted to sort of try and build that network, and we have a lot of health professionals that are keen on being able to, you know, integrate sort of stroke survivors into the community, especially young stroke survivors.
Saran 34:27
Because basically, with have so much life to live. Yeah, so that’s sort of that’s what Yes SA is and is trying to do. We’re trying to get funding but we’re also sort of being able to deal with stroke, which has now been sort of taken over by a hospital research group. And so sort of building up the raising the awareness of young stroke that way, right?
Saran 34:53
Okay. So what kind of events do you guys do you guys run events or how does that work?
Saran Chamberlain Reaching Out To Other Stroke Survivors
Saran 34:58
So we don’t at the moment. I want to be honest, I’m doing a lot of ones finding, you know, stroke survivors. There’s a lot of us, but I think what it is that we’re also sitting and I did the same for the first four years sit on the outside and kind of just wait for something that we kind of go, Yeah, okay, we’re comfortable to put ourselves in that vulnerable position.
Saran 35:22
So, I’ve met a lot of people working with stroke foundations, young stroke projects, but through researchers through clinicians in South Australia, because I’ve basically been around, and I’ve always sort of tried to give every sort of therapy ago, I’m known fairly well.
Saran 35:40
So people will sort of say, look, I’ve got a younger stroke survivor, who, you know, really nice to talk to someone. So I sort of start-up communication that way. And so we keep in contact and give them some opportunities to catch up. You know, there’s, we had like a group of eight that are all active on Messenger.
Saran 36:01
But then when we want to sort of catch up, there’s only two of us. You know, it just sort of happens. But yeah, we just sort of try. I’m just sort of trying to keep everyone up to date. And when people want to step in and are ready to, you know, actually get involved. Like it took me ages, I didn’t want to see myself as disabled.
Saran 36:24
I didn’t want to have anything to do with other stroke survivors took me five years, before I even got involved with Genius. And yeah, because I wanted nothing to do with people. So I get where people are at. And I sort of look at it and think, Well, I’m here, you know, when you want to get involved. I’m here.
Saran 36:48
So you were in denial?
Saran 36:51
Oh, yeah in denial. And so I was just moving forward. But I was not. I didn’t see myself as disabled. Because I kept working. Stupidly, I went back to work fairly quickly. And just was driving myself into the ground, and then starting other things, but just kept going. Because that identity sort of crisis, I suppose was there. Who am I post-stroke? But yeah, it was a denial, but it was still a positive denial. Like I don’t think I lost who I was but I didn’t realize that I was a stroke survivor.
Saran 37:37
Yeah. Positive. What’s positive about that? I suppose what’s positive about that is kind of you’ve faced it and dealt with it when the time was right. When you could face it and deal with it. That’s a positive. I mean, yeah, I like the way you spun it, right? Because usually, people see that as a negative, or they, think that it’s a negative they ah, they’re in denial, or they haven’t dealt with or they need to deal with it.
Bill Gasiamis 38:05
And people often sometimes get pushed to deal with stuff like that. And I can understand if you’re not ready to deal with it already because it takes them time and energy. And it requires you to go to new levels of learning. And that takes effort. And if that’s happening in the very early days for some people while they’re trying to raise their children, I can see how we could be interrupting their lives.
Bill Gasiamis 38:31
Because I had a similar very basic version of that very similar experience in that I didn’t want to go to rehabilitation anymore because it was taking up so much time in my life. And that meant that I couldn’t get back to the rest of my life. Three days a week, one hour a day wasn’t enough, but it took me an hour to get there an hour to do this session an hour to get home.
Bill Gasiamis 39:00
And it starts in the middle of the day or you know, 10 o’clock or whatever. And there’s your whole day gone, and you can’t go and do anything else with it. And at the end, after about six or seven months, I said to the guys, look, you guys are sacked. I’m not. I’m not coming back. I don’t need you anymore.
Bill Gasiamis 39:18
I’m going to take responsibility for my recovery from here on and I’m going to do the way that I want to. Not that they haven’t been supportive or helpful. It’s just that it’s inconvenient. And that was so difficult for me to have to deal with. And at that time, I couldn’t deal with the psychological and emotional impact of stroke.
Bill Gasiamis 39:38
I couldn’t go to my counselor I couldn’t go to wherever else I needed to go. I couldn’t read study or listen to a podcast. It was consumed by this effort to get to these rehabilitation sessions. And I couldn’t make it it was very difficult to make time for Not to make time to remember appointments, even though I had them in my calendar.
Bill Gasiamis 40:07
Even though I had set reminders, it wouldn’t occur to me when I was getting the reminders that that was a reminder about an appointment that was coming up in an hour or two, I was playing this weird game of setting reminders and reading the reminders, and not knowing that I needed to then take action on that reminder, and go and do something.
Bill Gasiamis 40:28
So I get what you’re saying about trying to or putting off dealing with the stroke. For five years, the question I have for you is, once you dealt with it, once you said, Okay, I’m going to take a step to accept this, then what changed for the positive in your life, I imagine that shifted things a lot.
Saran 40:56
So where you’re saying that you didn’t want to do therapy, what’s funny, as I’m thinking about it is that therapy just became my everyday life, like I’ve been doing therapy, at least three times a week for the last nine years. And I’ve never thought of, I mean, like I’ve had breaks, because, you know, you sort of need to mix it up and that kind of thing.
Saran 41:18
But my therapy was always that to try and sort of strengthen myself, you know, so that I was able-bodied, and I was able to sort of get around with my kids and, and make sure that I could, you know, stay up and upright, literally, in most cases, I think when I had faced it. I think because I still, as I said, you know, it was still positive and moving forward kind of momentum.
Saran 41:48
It just probably put pieces into place a bit more. So there were sort of just disjointed bits and pieces, I was just still just chugging along and, you know, whereas when I sort of went, right, well hang on, I’m never going to be able to run again, which is probably not, you know, wasn’t a goal.
Saran 42:12
But, you know, I’m never gonna have my hand back again. You know, I’m, I’m potentially going to always be one-handed. And, you know, and this is this is it. It wasn’t it was just, I think it was an acceptance of okay. Alright, then. So I’ve been doing all the, you know, I’ve been talking the talk, not walking the walk.
Saran 42:45
So I’ve been saying, Yeah, I’ll be fine. I’ll be fine. And then actually, Ah, wait, now I am feeling that, you know, I’m feeling okay. I think, certainly, from talking to other people, I think it was probably a little bit different because mine was more in a positive aspect.
Saran 43:10
And that denial was a small part of me and who I become, I suppose what that acceptance had become, was that I wanted to be able to my idea of raising awareness and supporting became, I started trying to connect with other people to say, Hey, it’s okay. You know, to try and make people’s journeys shorter and easier than mine was.
Saran Chamberlain’s Identity
Saran 43:41
That’s pretty good. Was it also an identity issue? So say, I’ll throw it out here, hypothetically. And maybe you relate it to this or you don’t. Was it? To be a mum and raise my children? I can’t be a stroke survivor. And then was it maybe a shift towards I’m a mum, but I can also be a stroke survivor and a mum?
Bill Gasiamis 44:07
And, therefore your identity is not lost or parked or made or altered? It’s just given an additional bit of information that you can add to it rather than it taking away from your identity. Does that make sense?
Saran 44:27
Yeah, yep. My identity for me was working. I didn’t have anything if I didn’t work. And so it was when I sort of found myself out of work that I realized that I was still something. You know, when I found myself out of work, I thought, right, that’s great. Nothing. Now what, but nothing changed.
Saran 44:51
You know, nothing changed apart from I had less stress about the expectations that I had at work. And so as soon like, I can still be this and I can probably be way better at being a mum, like, or being more present and doing things because you know, my identity of trying to do this work, which was always trying to, I don’t know, not only justify in myself but also justify my work with other people.
Saran 45:24
Suddenly, that wasn’t there anymore. So it was the case of why I can be a mum, and I can be a stroke survivor and so that’s where I kind of went, you know what I want to be in the stroke community, I want to be able to, you know, help people, I want to raise awareness, I want to be involved in research because far out like, I have this denial of being involved in it. But there’s so much here, there’s so much.
Bill Gasiamis 45:55
Work, work to be done. That’s kind of how I landed in the podcast, it was a bit selfish at the beginning, it was about me, was really about meeting other people. But it was trying to find people who understood me. And then I became embedded. And once you’re embedded, it’s hard to get out.
Bill Gasiamis 46:16
And not that I want to get out. But it’s a topic I’m becoming an expert on and I can, you know, talk about stroke, from the perspective of somebody who has spoken to 180 people that have had a stroke and interviewed them, you know, and that gives you a lot of insight.
Bill Gasiamis 46:33
It allows me to take a conversation and guide it towards making people aware of things that they weren’t aware of before, especially around identity and goal setting, and around all those things that are related, to those shifts that are thrust upon us, when we have a stroke, you know, it’s not our choice.
Bill Gasiamis 46:55
Things just change, and then we kind of have to sink or swim. So I think, for me, is the work there. And what I love about my work is it’s far-reaching. If it was on one, it’s certainly there’s an amount of there’s an amount of satisfaction to that, of course, absolutely right.
Bill Gasiamis 47:19
But because I can have them on-one conversation with you, and then I know it goes out to the podcast world, then I know that I’m doing one hour’s worth of work here, but it’s gaining 1000s of hours, potentially, of traction out there. And I could never get in front of 1000s and 1000s of people at any one time, I can’t do that I can only do that one-on-one most of the time unless I’m speaking to a crowd.
Bill Gasiamis 47:48
But even then most of them are not strike survivors. If I go to an event where I’m presenting, they aren’t all stroke survivors. And even that’s good, but that the message doesn’t filter through to the stroke survivors from the non-stroke survivors that don’t have the know-how the knowledge to, you know, filter the message through that I’m trying to send, hopefully, it applies to their life.
Bill Gasiamis 48:12
And one day Touchwood if they ever become unwell with stroke or something else, they’ll be able to remember the conversation and help hopefully it guide them. But that the work to be done is immense. And one of my mates kind of gave me that insight. So where do you want to do your work and present?
Bill Gasiamis 48:34
And who do you want to coach and speak to? And I was like, I live in Preston in Melbourne, Victoria, you know, and it’s like, that’ll be good. Preston won’t be good. It goes well, like there’s more to the world than just Preston Victoria, you know that? Yeah. I’m like, yeah, and now what’s your point? Wouldn’t it be great to just work with people anywhere and everywhere?
Bill Gasiamis 48:54
How would you find them? How would you reach them? And that’s when the idea came, oh okay maybe I could do something broader than that. How would I do that? And then the podcast was the only real solution to that. And then whoever wants to do it can reach out to me and work with me directly if that’s what they choose to do, rather than me knocking on doors, like a Sunday Bible basher. All I had to do was put it out there. And then if people want to come they come to me.
Saran 49:29
And I feel as though people are slowly learning the real value of the lived experience. voiced, and you know, and we can see that in Stroke Foundation, with the young stroke project and when I was employed as the engagement project coordinator, because they couldn’t, you know, that nonbiased, conversation that we can easily have and we don’t if I say I’m fatigued, you you say, Oh, I have an app during the day too, it’s not the same thing.
Saran 50:03
You know or sensory overload, or you know, sometimes my ears ring as well, that is not the same. You know, there’s that kind of thing that really, it’s something that, again, we would not want anyone to have at all, if we could have the choice, but, you know, it’s knowledge.
Saran 50:25
And it’s something that people just don’t get. And so that’s why we can add that value if we speak with either researchers or clinicians or anything like that. And that’s sort of what I’m bashing through as well, which is great. Yeah, and because in some ways I kind of went, I’m a bit of a smartass, I kind of go it’s not like they can argue with me that they can’t go, Hey, that’s not how you feel? Because kind of Oh, actually, yeah, it is.
Saran 50:55
Yeah, there, there is a little bit of the blind spots that people will have even people who’ve worked with stroke survivors a long time, and that’s okay, I get it. Now, I was frustrated, and annoyed about it. Early on, but I understand why it is like that. And there’s no issue now.
Someone On The Inside
Bill Gasiamis 51:15
But that’s why I get excited. Which is weird. When I find a doctor who’s had a stroke. I don’t want them to have had a stroke, I don’t want it but the one I was like, I, okay, a medical person who’s had a stroke. Now, we’re kind of starting to break new territory, and we’re starting to get a person who’s on the inside, who knows what it’s like to be us, to go through what we went through.
Bill Gasiamis 51:46
And that informs far better outcomes and conversations with the people that they work with that matter. I’ve interviewed several people who have been doctors, psychologists, that kind of stuff who have had a stroke, and therefore have been able to just have a better what’s the word like a better impact on their colleagues about how to deal with somebody in that space? It’s that lived experience from a colleague of theirs.
Bill Gasiamis 52:22
And then that just takes things to a different level. You know, imagine being a stroke survivor, who’s taught psychologists because you’re a psychologist, and you know, the language and how they speak, who are treating stroke survivors in hospital as part of their stay or in as part of their rehabilitation? If they’re struggling psychologically, I mean, that would be a far richer kind of recovery or way to experience psychology, I suppose.
Saran 52:59
Yes, yeah. Again, it’s not something that we would wish on anyone, but it’s, it’s a hell of a lot of value when we do find someone, isn’t it?
Saran 53:08
Yeah. And whether they’re an occupational therapist, a doctor, or a GP doesn’t matter who. And that’s why I think Jill Bolte Taylor, is someone who gets a lot of air time because she’s written amazing books and took her brain onto a stage once.
Bill Gasiamis 53:29
But also because she was a neuroscientist studying, you know, brain conditions. And then she had her own experience. And then she was able to tell that story from a scientist’s perspective, as well as a stroke survivor’s perspective is just next level and such a unique gift to be able to have and share, even though you wouldn’t want them to ever have a
Saran 53:54
Yeah, that’s right. Again, making the most and that sort of, not that I’m Jill Bolte Taylor’s level at all, but I’m making the most of what I’ve got. And I’ve made the most of the experience that I’ve had. And you know, and I think that, yeah, I feel as though if I can connect to people and help people in any certain way and not from a selfish level, just like, I just wish that someone had maybe spoken to me when I was there, that would be great.
Saran 54:31
And 10 years ago, it was so different. It’s not that long, but it was so different. We didn’t have podcasts. We didn’t have YouTube, we didn’t have any of that stuff where it’s there’s nothing, almost nothing where things were proliferating to this level. And yeah, it was kind of like a dead zone of information.
Bill Gasiamis 54:48
And if you didn’t get it at the hospital, you might not have got it at all. And if you didn’t Fluke upon the Stroke Foundation, which I did, you wouldn’t have got anything. I was in hospice Close for, you know, more than three years and in and outs, right? Yeah. And I didn’t know that my hemorrhage was regarded as a stroke.
Bill Gasiamis 55:13
I didn’t know that I, I learned that very late on in that journey. And then when I find a letter, I was like, Ah, crap. That’s why I can relate to other people who have had a stroke because it’s a bloody stroke. It just is a blade. It’s not the other kind. And it’s like, right, okay, now I know what’s happened to me, I get it. Nobody said it, nobody said that.
Bill Gasiamis 55:41
They said you had an AVM, which is worse than blood in your brain. They also said to me, the AVM is technically a tumor. So the bleed was within the tumor, which is within your brain. So that gave me all this technical jargon and a battle complicated. And that’s why I never got dealt with by a stroke department.
Bill Gasiamis 55:59
That’s why I never was given any information about the Stroke Foundation because that exact word in my diagnosis wasn’t part of my diagnosis. Therefore, they never sort of mentioned that. It was just nuts. Certainly 10 years ago, but it was like another time in the world.
Bill Gasiamis 56:20
It was like a completely different time in the world was nuts. And I think that’s kind of what spurred me on to, to meet other people and to find other people was like, what else? Do I need to know that? I don’t know. That they’re not telling me? That’s gonna like make my life easier?
Saran 56:38
Yeah. I started. And only just recently, I must admit, I’m still learning. Going on to Instagram, I’ve got I’ve got a baby scram. They’re just sort of sharing my stories. And it’s weird. Like, you know, again, I was not there. I mean, there was no real social media when I had the stroke.
Saran 56:58
But the amount of people that have seen it now it’s just like, Oh, my God, there’s so many people out there who had strokes on Instagram. And you think, Wow, that’s fantastic. Like, why don’t you know, and I sort of dwell on it. But if you do go find out, that would have been so good way back then.
Saran 57:16
But, yeah. And the amount of people that want that engagement straight up, you know, because, this is, this is how we work. This is how we communicate, we don’t need to have, you know, we don’t need a phone, we don’t need, you know, we don’t need a telephone book, where, you know, it’s all there at our fingertips. And I think that that’s amazing.
All About Stroke
Saran 57:37
I’ve got about 4800 followers on Instagram, they’re all stroke survivors. When we interact on Instagram, it’s a proper discussion about stroke. It’s not about what he voted for or what you believe in, or any of that bullshit. So that’s great. Yeah. You know, it’s sharing the podcast, and then getting people to interact and all that type of stuff. And then the podcast gets downloaded about 4000 times a month from all over the world.
Bill Gasiamis 58:13
You know, so you know, it’s a proper amount of, what’s the word lack of impact, or I don’t know what the word is, and then every day or every second day, or, you know, somebody contacts me to say something about someone that’s had a stroke, or they’ve had a stroke or a podcast, they listen to, you know, or a caregiver or whatever.
Bill Gasiamis 58:42
All the time. And it’s like, okay, well, how good is that? And, you know, they can be on the other side of the planet, and they can get to us immediately, and within moments, and we can respond immediately, and maybe help ease their suffering or their anxiety.
Saran 58:59
Just make them feel heard, that’s less alone. That’s the biggest thing is that you know, because you, do you, especially the way that, you know, maybe some medicos can sort of tell me about your stroke or not to have a stroke, as the case might be with you. You know, yeah, you sort of think, hang on.
Saran 59:22
This is weird. So does this mean that I’m the only one around but being able to speak to other people and see other people’s stories, I think makes that they expect acceptance, you know, or, you know, them to move forward rather than being stuck in that sort of position, or going backward? I certainly think it Yeah. It helps at some stage or another, whether or not it’s ready right then and there. That leaves no, it’s there. So I think that’s what’s good.
Saran 59:54
Yeah, that’s true. A lot of people will contact me and say, such and I know just had a stroke, or x Right. And I told them about you and I’m like, okay, it might be a while before they come around and need to speak to me specifically or anyone about what’s going on.
Bill Gasiamis 1:00:12
I know there was a girl I know who was found to have had an AVM who’s a member of some family of ours but from a different part of the family different side. She was in denial that she had an AVM for six to seven months, and she wasn’t ready to discuss it or talk about it or whatever until it got to the point where it kept bleeding.
Bill Gasiamis 1:00:36
And AVM is an arteriovenous malformation because it keeps bleeding. She eventually decided that she couldn’t avoid it. But it still took a long time for her to accept that. It even happened, let alone I’ve got to do something about it and speak to Bill is kind of like was not even in the picture.
Bill Gasiamis 1:00:59
It’s like maybe there was a bit of denial. I don’t know what it was fear or whatever. But yeah, people have a different journey to being ready to experience feedback or information or even know what questions to ask takes some time to develop them in your head.
Saran 1:01:19
Yeah. Yeah. Everyone’s on their journey. As long as we’re all sort of there around to Yeah, for that. That’s what I want to do.
Bill Gasiamis 1:01:34
Yeah. Yeah. It’s brilliant. Now where can people find out a little bit more about the stuff that you do in your organization?
Saran 1:01:46
So, I mean, my website is yesssa.com.au. But I’m also on Facebook, and our Instagram. So my actual Instagram handle is Young Stroke Journey Stories. Yeah, I mean, I’m also mainly Facebook and Instagram, I think, is sort of where I am. The website, you know, Facebook is fairly big I think, for my age being 40 on Instagram I hear better for younger, I’m so old. You know, but I’m, I think that’s sort of really the main social media that I’m on.
Bill Gasiamis 1:02:35
If you’re so old in your 40s, like me, what are you going to be when you’re in your 80s?
Saran 1:02:43
I’m gonna be a lot wiser.
Bill Gasiamis 1:02:47
A fossil, or something else? Look, thanks so much for being on the podcast and sharing your story. I appreciated our chat getting to know you a little bit and sharing your story. And hopefully, people listening find it relatable, and they’re able to take a little bit out of this. And it’s a great thing that you’re doing.
Saran 1:03:11
It was great chatting with you.
Bill Gasiamis 1:03:13
Well, thanks for joining us on today’s episode. I hope you enjoyed the conversation and got something positive from it. Please like comment and share this episode, and give the episode a thumbs up if you’re on social media. Or if you’re watching on YouTube. Leave a comment on every interaction that you do or that you leave the show helps other people find it easier online and it also helps the show rank better on the search engines.
Bill Gasiamis 1:03:44
As a result, hopefully, what that means is that more stroke survivors and their caregivers from around the world will find the show easier. And that will hopefully help them have a bit of stroke recovery. And get in touch and find immediately other people that are like them, so that they can have perhaps less anxiety and worry about what it is that they’ve experienced and what the future holds for them. So once again, thanks for listening. I appreciate it and see you on the next episode.
Intro 1:04:15
Importantly, we present many podcasts designed to give you an insight and understanding into the experiences of other individuals’ opinions and treatment protocols disgusting any podcast or the individual’s own experience and we do not necessarily share the same opinion nor do we recommend any treatment protocol discussed.
Intro 1:04:32
All content on this website at any linked blog, podcast, or video material controlled by this website or content is created and produced for informational purposes only and is largely based on the personal experience of Bill Gasiamis the content is intended to complement your medical treatment and support healing is not intended to be a substitute for professional medical advice and should not be relied on as health advice.
Intro 1:04:54
The information is general and may not be suitable for your injuries, circumstances or health Do not use our content as a standalone resource to diagnose, treat, cure, or prevent any disease for therapeutic purposes or as a substitute for the advice of a health professional.
Intro 1:05:09
Never delay seeking advice or disregard the advice of a medical professional, your doctor, or your rehabilitation program based on our content. If you have any questions or concerns about your health or medical condition, please seek guidance from a doctor or other medical professional.
Intro 1:05:23
If you are experiencing a health emergency or think you might be, call Triple Zero in Australia or your local emergency number immediately for emergency assistance or go to the nearest hospital emergency department medical information changes constantly. While we aim to provide current quality information in our content.
Intro 1:05:39
We do not provide any guarantees and assume no legal liability or responsibility for the accuracy, currency, or completeness of the content. If you choose to rely on any information within our content, you do so solely at your own risk. We are careful with the links we provide however third-party links from our website are followed at your own risk and we are not responsible for any information you find there.






