20-year-old Jessica Lepper suffered from a ruptured AVM on her shift in a hospital as a nurse about a year ago. She is now also dealing with epilepsy caused by her stroke.
Instagram: www.instagram.com/jessicasavmjourney/
00:29 Introduction
03:17 Jessica had a ruptured AVM
09:10 Physical challenges after the surgery
11:47 Having epilepsy while in AVM recovery
15:18 Having Gamma Knife to remove the AVM
20:08 Sharing scars
Highlights:
Jessica 0:00
But I noticed I couldn’t read or anything like that. My right side was quite weak. So I couldn’t hold a glass or anything like that. I couldn’t move it, but yeah, and I couldn’t walk at all.
Intro 0:22
This is recovery after stroke with Bill Gasiamis helping you go from where you are to where you’d rather be.
Introduction

Bill 0:29
Bill Gasiamis here this is Episode 96 and my guest today is Jessica Lepper. Jessica was a 20-year-old nurse on shift in a hospital when she noticed herself not being able to speak due to a ruptured AVM. Since then Jessica has had to overcome a lot to get back to work and is now being monitored due to seizures.
Bill 0:53
Now just before we get started with the interview, I wanted to thank everyone who reached out to me to send me lovely feedback. And to share how much each episode has helped them or made a difference in their life. It’s so heartwarming to hear from you. And if you felt like reaching out before, but you haven’t yet, I’d love to hear from you.
Bill 1:14
This podcast is for you and me and I do this work because I love what I get from it, I get so much satisfaction and it makes my life better. And that’s why the podcast exists. And I hope that that’s what it does for you. If you feel like shit from time to time, I hope that it makes you feel better. If you are feeling alone, I hope that it makes you feel somehow more connected.
Bill 1:38
If you feel isolated, you’re not alone. Just reach out. You can send me an email at [email protected] I answer all my emails personally. Also, if you love the recovery after stroke podcast and you think it’s helpful, please share it and tell others about the podcasts so that they might benefit too.
Bill 1:58
If you’re watching on YouTube, please give us a thumbs up and leave a comment. I love to hear from other stroke survivors. And again, I answer all my comments personally, go to iTunes or your favorite podcast app and also give us a five-star review there. That’ll help search engines find a better one and put it out to more people.
Bill 2:18
Also, if you want to follow me on Instagram, just go to Instagram.com/recoveryafterstroke or Facebook.com/recoveryafterstroke. Finally, I wanted to let you know that you can now also download all the words of each episode as a PDF. It’s perfect for you if you prefer to read and take notes or highlight different parts of the interview for future reference.
Bill 2:43
It’s a great way to learn and it helps retain new information to memory. Just go to recoveryafterstroke.com. Click the image of the episode you’ve just listened to. At the very beginning of the page, you’ll see a button that says Download transcript. Click the button enter your email address and the PDF will begin downloading. Now it’s on with the show, Jess Lepper welcome to the podcast.
Jessica 3:07
Hi.
Bill 3:08
Hi Jess, thanks so much for being on the podcast. I appreciate it. Can we just start with you telling us a little bit about what happened to you?
Jessica had a ruptured AVM
Jessica 3:17
Yeah, sure. Um, so long story short, I was a nurse at a hospital in London. And I was just talking to a patient and my words started to slur and then I completely lost my voice. And I thought that a bit weird, and then I got sent to Charing Cross, which is a neurological center in London. They confirmed that I had an AVM rupture, which caused me to have a stroke.
Bill 3:50
Wow, how old were you at the time?
Jessica 3:53
22. So quite young. I think that’s why we didn’t know what was going on.
Bill 3:59
Were you with professional people around there? Were there other nurses and doctors around at the time that I happened?
Jessica 4:09
Yeah, I was so lucky. Yeah.
Bill 4:13
Do you have any recollection of after you couldn’t speak? What was the what am I trying to say? Like I’m trying to say did you notice yourself not being able to speak?
Jessica 4:28
Yeah, I think I was thinking what I was trying to say but I there was no word coming out. Really? Yeah.
Bill 4:40
So you were at the hospital for work. You had an AVM rupture and you found yourself being in the best place at the right time. Was it a CT scan immediately what happened after that?
Jessica 4:56
Yeah, so I went downstairs for AA and they rushed me and I was like, This is so like weird and they rushed me in an ambulance to the neurological center. And I had a CT scan straightaway and yeah confirms a stroke or brain hemorrhage.
Bill 5:18
Wow, what happened after that? What was the process that they took you through?
Jessica 5:23
And they started me on Keppra which is a seizure meds, just in case I had a seizure. And I was bedbound They said like, I can’t move or anything. And then I was sent up to the neurological wards. And then yeah, that’s where the story starts really.
Bill 5:47
Did you have surgery after that?
Jessica 5:48
Yeah, I did. Um, I had a craniotomy to remove the AVM. And it didn’t go to plan to be honest. The operation was meant to take about five hours. But I had a hemorrhage on the table again. So it took about nine hours. And I ended up in ITU. And the surgeon straight to my parents and said like, he wasn’t sure how my condition would be. He said, like, I probably won’t walk talk like, I’m probably not going to be as normal as I was before which.
Bill 6:38
Wow. So when you work up, How long after your surgery? Do you have any recollection of how long it was? After you kind of woke up and started to realize that you were in a hospital bed?
Jessica 6:51
I woke up and I just saw my parents waving through the door and then That’s it. That’s all I can remember. The ICU experience. I can’t remember to be honest.
Bill 7:07
Yeah. Wow, that is fascinating before the stroke happened or before the hemorrhage occurred. Were there any signs leading up to that day to go to work? Did you have any idea that perhaps there was something serious going on in your body?
Jessica 7:26
No, so I was in Australia 73 hours before that, and living my life like living the dream. And then I went home to Devon, no sign of anything, and then ready to work fine. And then suddenly that was it, it’s so weird.
Bill 7:44
So unexpected and so young, and everybody’s going, everyone’s probably freaking out. How did your family cope with all this sudden drama and emergency?
Jessica 7:57
Well, they live in Devon which is about four or five hours away from London and they got the call and I think they didn’t know the situation until they got there and they were all like really positive and you know kept me positive and didn’t stress me out but I think behind the scenes everyone was pretty stressed out.
Bill 8:28
You woke up from surgery what did you notice about what was different about your body? Did you have any idea of what was different from what was happening to you?
Jessica 8:40
I’m not, to be honest, My speech wasn’t changed. So it was quite minimal, but I would still like to do some hand actions. But I noticed I couldn’t read or anything like that.
Bill 9:03
Did you have any problems walking any numbness in any one of your limbs or anything like that?
Physical challenges after the surgery

Jessica 9:10
My right side was um, yeah, quite weak. So I couldn’t hold a glass or anything like that. I could move it. But yeah, and I couldn’t walk at all.
Bill 9:26
Did you have to have rehabilitation as a result of that?
Jessica 9:30
Yeah, physio which was quite hard because I probably was bed-bound for like two weeks, because I had to, obviously do my ITU experience, which is like a week and then it was moved to HDU. And then I was bed-bound and then the physio started getting me up, but it was a nightmare.
Bill 9:55
What’s, it u and H GG?
Jessica 9:58
Oh, sorry, intensive care sorry.
Bill 10:02
And HDU is?
Jessica 10:04
High dependency. It’s just a step down from ITU.
Bill 10:12
Right. Okay. So then, did you have some time and rehabilitation was it two weeks in rehabilitation?
Jessica 10:20
And so I probably spent four weeks on high dependency. And then I had speech and language every day. The occupational therapists showed me quite a lot because my short-term memory was like, literally gone. I couldn’t remember anything.
Bill 10:42
Wow, how long ago was this now? So we’re in? It’s April 2020. And when did this all happen?
Jessica 10:52
January 31, 2019. Yeah, so last year.
Bill 10:57
It’s been a year.
Jessica 10:59
Yeah, I’m so lucky, to be honest. But yeah.
Bill 11:02
Yeah, we are. What were the main things that you had to relearn how to do again?
Jessica 11:10
I guess my speech was one of the main things, and I probably still struggle with that at times, especially when I’m tired. So when I went home from the hospital, I had like intensive speech and language for quite a long time. And yeah, which was tricky at times, but we got through it.
Bill 11:34
Yeah, what did it mean for your driving and just being a normal person you know daily, what did that mean for what you could no longer do?
Having epilepsy while in AVM recovery
Jessica 11:47
And so I couldn’t drive. And I now have epilepsy as a consequence. So I can’t drive at all now until I didn’t have a seizure for a year.
Bill 12:01
And is the epilepsy. Something that you notice coming on? Is it something serious that occurs? Or is it something that you can manage and control when you become aware of it?
Jessica 12:12
And to be honest, I get no signs at all. And so I just like fall on the floor (inaudible) remember really.
Bill 12:23
Wow and you fall on the floor have you hurt yourself doing that at all?
Jessica 12:27
The first time? Yeah, I did. But I can usually manage to get on the floor. I have like five seconds and then it all starts.
Bill 12:38
And then you need people around you to help you recover from that. How does that work?
Jessica 12:46
So usually, it’s like an ambulance has to come because they last like 40 minutes. It’s not like a quick like two minutes or anything is quite intense.
Bill 12:57
Right. Does it require hospitalization as well?
Jessica 13:01
Yeah.
Bill 13:04
Wow, so you’ve been through quite a tough time. And it seems like you’re still going through a tough time. Is it getting better? What are you noticing? what’s getting better for you?
Jessica 13:15
Yeah, definitely. My speech is like, if you didn’t know me, you probably think like, I’m just a normal person. And this is my speech. And I have to think about what I’ve been saying. And sometimes the words don’t come out. My walking’s fine. I’m so lucky with that. And, it’s just the epilepsy and speech really, that have been affected. But yeah.
Bill 13:47
Have you been able to get back to work as a result of the time that’s passed since you’ve had a stroke or are you not back at work yet?
Jessica 13:57
I went back to work on February 3rd so basically a year after my stroke, as a nurse, but, with this situation going on, I’m back in Devon, for now, and then we’ll see what happens.
Bill 14:14
How do you find being back at work? Now that you’re a stroke survivor? You’re somebody who’s got a real experience of something really dramatic, even at the age of 22. How did you find going back to work?
Jessica 14:31
I was relieved to be back because, to be honest, we didn’t think I’d ever work again. And I was when I was with the same teams, everyone knew me and I had a lot of visitors during my time, like in the flat and Wimbledon, so everyone knew the situation. We’re helpful. It’s a bit weird going back to the place it happened. I’m, sorry that took me a while but other than that, I also forgot that the AVM wasn’t completely removed. So I had to have a Gamma Knife. I don’t know if you know what that is.
Gamma Knife to remove the AVM
 Bill 15:18
Bill 15:18
Tell me a little bit about that is that radiation?
Jessica 15:23
Yeah it’s radiation just to zap away the AVM hopefully, but it works slowly so it probably takes about five years and then we’ll have to see whether it’s working
Bill 15:40
And you have to have ongoing Gamma Knife procedures?
Jessica 15:47
So after five years, they’ll do an angiogram and then we’ll see how it is and if it’s still there, then we’ll have to do another cycle. But hopefully, it won’t be there.
Bill 16:03
Fingers crossed. So what happened with the surgery though? So you still had a craniotomy? I saw the scar on Instagram that’s quite an awesome scar.
Jessica 16:11
Yeah, crazy.
Bill 16:12
What was the outcome of the surgery? What did that achieve?
Jessica 16:19
So that was hopefully to remove the AVM, but it was too deep. So they’ve removed quite a lot of it. But some of it remains.
Bill 16:33
Right. Okay. So they’ve gone in and they’ve decided to not go any further and then leave it be, get you out of the hospital get you recovering, and then treat it with a gamma knife. So that it’s less in weight is that right?
Jessica 16:50
Yeah, you’re right. You’re right.
Bill 16:52
Now, tell me this whole experience has made you a better nurse.
Jessica 16:58
Yeah, I think Yeah. It makes you think you empathize more. And you think about things like, you know, the parents and how they’re feeling because sometimes you just, you know, so busy, you just get on with it and you’re just focusing on the child, but actually, you need to focus on the parent as well. Because if they’re not positive and, you know, resilient, then the child is not going to get better. As soon as like as quickly.
Bill 17:31
You’re a nurse and you have all this inside information about medical stuff. Does that make you feel better about what you’ve learned about your experience? Or because you know what, you know, does it give you some kind of a sense of underlying concern?
Jessica 17:49
No, I think during the whole experience, obviously I knew, like my observations and whether they were normal or not, but that was made me, It made me understand the situation more, I think. Because obviously, I knew what was going on really, because some people obviously wouldn’t know.
Bill 18:15
They wouldn’t have a clue. I’m the kind of guy that needs a whole bunch of information. I need to know everything I need to ask all the questions, whether it’s good or bad. Do you find that being a nurse gave you that opportunity to be in control of a little bit of the information? And is that a good thing for you?
Jessica 18:34
I think because at the time I can speak it’s quite frustrating. After all, I wanted to know, like you said, everything that was going on, but I couldn’t express myself. So we had like a word board to try and I could throw the things I wanted to say but obviously, if it’s quite complex then obviously, I could have.
Bill 19:00
Yeah, then it becomes harder to communicate what you want and it takes a lot longer. So what were some of the things that you wanted to communicate that you couldn’t get the message across?
Jessica 19:13
I guess as a nurse, I wanted to know, the jobs and you know the dosages and stuff like that. I couldn’t ask that.
Bill 19:23
Yeah, why did you feel you needed to know the type of medication you’re on and the doses?
Jessica 19:31
I think because like the Keppra and stuff that is like an anti-seizure one. And obviously, I know like you steroids and stuff like that, obviously that I was on by just wanting to know the dose because obviously, I know how like, serious it is or not, not as serious.
Bill 19:51
Yeah, I see what you’re saying. Now as a girl with beautiful blonde hair and long hair, how did you deal with the whole they’re going to cut my hair situation, or were you aware of that? Or did you kind of work that out later? And then
Sharing scars after stroke

Jessica 20:08
Yeah, I think, yeah, it’s one of those things you just have to get over, don’t you? I think, you know, we had to do the surgery. Otherwise, I’d probably have another stroke. So we just thought we’ve got to get on with it. And I can cover up so yeah, it’s gone now. So that’s good.
Bill 20:25
So what did they do just take out the bit that they were going to do the incision on?
Jessica 20:30
Yes, the surgeon was really good. He just literally did it from here, back to my ear and that’s it. He didn’t like to shave, anything that didn’t need to be shaved. So got quite lucky.
Bill 20:44
I got to prepare myself for the surgery. I was told that we were going to have surgery on this particular day. So I went and got the hairdresser to give me a number zero like basically what I’ve got now but completely bald. The funniest thing happened because it was a, I think it wasn’t Zero number one. It was short everywhere.
Bill 21:11
And then it was shaved in the area where they opened my head up. And then as it started to grow back, I had this really weird look. It was kind of long, and then it had like a line. And it looked bizarre. So four days after my surgery, I had to shave it again. So I don’t look too silly.
Jessica 21:34
How is yours healed?
Bill 21:36
Yeah, it’s healed. Amazing. It’s been four years or so. And you can’t see it at all.
Jessica 21:47
No, not at all.
Bill 21:49
If I cut my hair short, where from time to time I do. You can see it. It does come through but not a lot. The hair has mainly grown back.
Jessica 21:59
Oh, that’s good.
Bill 22:02
So with you is it visible that all or only when you move your hair?
Jessica 22:08
Just when I move my hair back which if you didn’t know you just think it’s a little bit bald you know which you know people have so yeah, I’m quite lucky.
Bill 22:19
For different reasons. Yeah.
Jessica 22:21
Yeah, exactly.
Bill 22:23
So tell me about the next few years What are they like for you What have you got planned to do and achieve?
Jessica 22:32
I think just to get my new normal routine back obviously, I was living in Devon until like six months last year. I’m just getting used to being in the flat on my own because I don’t like to be on my own now. We’ve got an alarm fitted so I can press it if I need any assistance. And then just seeing how it goes really and to be honest.
Bill 23:02
Has it impacted your relationships with your friends? Or did you have a boyfriend or a partner or anything like that?
Jessica 23:11
With my friends, they’re amazing. I think it brought us all closer, to be honest. Because at times at least you realize who’s there, don’t you? And I’m sure you realize that too.
Bill 23:23
Yeah. I think one of the biggest things that happened to me was I realized who were the ones that would say something like, if there’s anything you need, let me know. And when I asked for their help, they stepped up and made a difference. They surprised me. But when I asked them, they said yes. Did you find that as well?
Jessica 23:50
Yeah, definitely. And just from their being in the house and the flat and stuff like that. It made my communication better because I was always talking in communicating with someone other than my family. So that was good actually.
Bill 24:08
Yeah, were you with a partner at the time?
Intro 24:10
If you’ve had a stroke, and you’re in recovery, you’ll know what a scary and confusing time it can be, you’re likely to have a lot of questions going through your mind. Like, how long will it take to recover? Will I recover? What things should I avoid? In case I make matters worse, doctors will explain things. But, because you’ve never had a stroke before, you probably don’t know what questions to ask.
Intro 24:36
If this is you, you may miss out on doing things that could help speed up your recovery. If you’re finding yourself in that situation, stop worrying, and head to recoveryafterstroke.com where you can download a guide that will help you it’s called Seven Questions to Ask Your Doctor about your Stroke.
Intro 24:55
These seven questions are the ones Bill wished he’d asked when he was recovering from a stroke. They’ll not only help you better understand your condition, they’ll help you take a more active role in your recovery. Head to the website now, recoveryafterstroke.com, and download the guide. It’s free.
Jessica 25:24
No. A bit since then, yeah.
Bill 25:27
Since then, so you’re living with somebody now? And how soon did you make him aware of what your challenges were?
Jessica 25:35
Well, he was just on the scene before, and then after the stroke, he didn’t see us for quite a while because everything was happening. And then, he was told quite a lot of things. But yeah, he doesn’t know when I have my Instagram account. Sometimes he’s like oh, that happened. And yeah, he didn’t know something.
Bill 26:04
So he’s just catching up on all of the juicy details now rather than earlier on.
Jessica 26:10
Yeah, you’re right.
Bill 26:13
Does he find it weird when you start a sentence and can’t get to the end of it when you forget what you’re going to say?
Jessica 26:19
No, he’s quite understanding to be honest. Yeah, definitely. Because I guess he knew he saw me at probably the worst of my speaking. So obviously is a lot better. Yeah.
Bill 26:31
Yeah, that’s awesome. How are you affected? Now? A lot of people that experienced a stroke experienced some kind of other challenges, you know, anxiety or things like that. Did you find any challenges with your mental health or anything like that?
Jessica 26:49
To be honest, I think I’m quite lucky. I think the only time that it is not able to go to things like nights out and stuff like that. I probably can’t do that anymore. But my friends are understanding and stuff like that. So I’m quite lucky and my family is supportive and, you know, they taught me to like me, like really positive and stuff like that. So, to be honest, that hasn’t affected me. At the moment. You never know what’s gonna happen to you. But yeah, at the moment, I’m all good. Thank you.
Bill 27:23
Awesome. And what’s interesting is that you’re not able to go out because of the stroke. And now none of us can go out because of this other thing that’s happening around the planet.
Jessica 27:33
I know it’s crazy, isn’t it?
Bill 27:34
It’s no real different, is it? However, tell me about your reason why you couldn’t go out at night. What was stopping you from being able to be out at a club for example?
Jessica 27:51
And because obviously with this epilepsy now I can’t drink and sometimes it’s my tiredness that affects me that’s when I have a fit. So I don’t want to risk it.
Bill 28:07
Yeah, so it’s better to be cautious. And do you find that lights or noise like that sound music that affects you?
Jessica 28:18
No not at all I’m quite lucky at the beginning like light is I hate I hated them sometimes. If I have liked the spotlight. I don’t like that. But other than that, yeah, I’m quite fine. Really? Yeah.
Bill 28:35
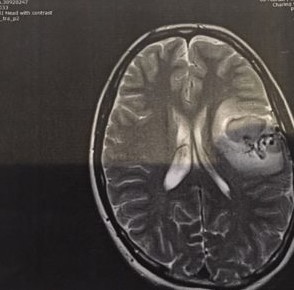
That’s amazing. I saw the scan on Instagram of the bleeding in your brain. That was quite (inaudible) taken up, right?
Jessica 28:45
Yeah.
Bill 28:48
Did that happen rapidly? Did it become that big that bleeds very rapidly?
Jessica 28:55
Huh? Yeah. So crazy. Like when you show a doctor Now they’re like God how do you survive that? Like, it’s crazy, isn’t it?
Bill 29:04
Yeah, it’s amazing. It just goes to show that every stroke is different, and every person is different. But there’s real hope in having a conversation with you and getting to know you a little bit. There’s such an amount of hope for people that are freshly going through this or have just, you know, who knows somebody who’s just gone through this.
Bill 29:25
Such a great amount of hope that people can work on recovering and getting better and getting back to some kind of a normal life. And now this experience, I wouldn’t wish it upon anybody. But isn’t that amazing that this experience that has happened to a nurse who’s 20-something years old can now support her in doing a better job? While she’s caring for other people?
Jessica 29:52
Yeah, it’s crazy, isn’t it? Yeah. And that’s why I want to create that Instagram account. Because you know, we need to be positive and you know, share our experiences. So, people, you’ve got to get through having you’ve got hope, and yeah.
Bill 30:11
So what do your family and parents think? are they keeping an eye on you? Are they fussing over you and how are they behaving now that it’s been a year that things are sort of starting to settle a little,
Jessica 30:23
and I think behind the scenes they’re probably a bit stressed, but they don’t show it at all. I think my mom probably worries about it more than my dad. Just cuz he’s like a chill person. We’re quite lucky.
Bill 30:39
Yeah, look, Jess, it’s been awesome to get to know you a little bit. I appreciate you being on the podcast and sharing your story. I wish you all the best with the recovery ongoing, and I think it’s gonna make you an amazing nurse next level. Amazing. And at such a young Age. I think it’s going to give you a lot of life experience early on and you’re going to be able to use that in a real positive way. Although I understand that it’s challenging and I would have much preferred not to be having a conversation with you about a stroke that you had.
Jessica 31:15
Yeah, thank you that’s kind.
Intro 31:19
Discover how to support your recovery after a stroke. Go to recoveryafterstroke.com






