Jessica Tagami was not surprised when her husband Phil experienced a stroke. On reflection, they both knew his work and sleep habits were unsustainable. Undiagnosed type 2 diabetes was the last straw.
Highlights:
03:53 The Stroke Symptoms
09:19 Progressive Stroke
14:53 Behavioral changes after stroke
22:09 Stroke recovery could be a lifelong journey
29:43 The 90-day stroke recovery period
41:46 About Diabetes and why it could lead to stroke
51:16 Becoming more compassionate after a stroke
57:58 Jessica’s art therapy
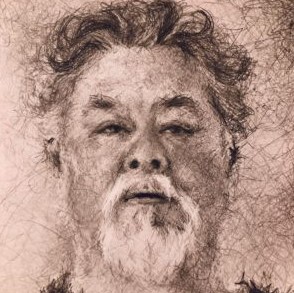
1:05:18 Phil’s portrait as a representation of his stroke experience
Transcript:
Jessica Tagami 0:00
He says that that’s so funny that you say that he’s noticed that a lot and he’s vocalized. But he’s like, I used to never pay attention to people who are walking with a cane or who needed extra time to cross the street. And now that’s all he sees.
Bill 0:14
Stroke has this way of making people more compassionate. Yeah. That’s a shit way to get too compassionate but it does do that.
Intro 0:26
This is recovery after a stroke with Bill Gasiamis. Helping you go from where you are to where you’d rather be.
Bill 0:33
Bill from recoveryafterstroke.com This is Episode 84. And my guest today is Jessica Tagami. Jessica is married to Phil who in his early 50s had undiagnosed type two diabetes, which revealed itself after he had a stroke. As a mom of two teenagers Jessica turned to ask to help her cope with the challenges stroke created for families.
Bill 0:57
Now, just before I get into my chat with Jessica I wanted to let you know that you can now download all the words of this episode as a PDF. It’s perfect for you. If you prefer to read and take notes or highlight different parts of the interview for future reference. It’s a great way to learn and it helps retain new information to memory. Just go to recoveryafterstroke.com. Click on the image of the episode you’ve just listened to.
Bill 1:23
At the very beginning of the page, you will see a button that says Download transcript. Click the button, enter your email address and the PDF will begin downloading. Also, a few weeks ago, I launched recovery after stroke coaching, The people who have signed up and are being coached by me and are being helped to overcome challenges, including fatigue, anger, isolation, amongst other things.
Bill 1:47
For 12 months of support, they paid only 149 US dollars. So if you’re a stroke survivor who wants to know how to heal your brain overcome fatigue and reduce anxiety Recovery After Stroke Coaching may be for you. If you have fallen in the cracks between hospital and home care, and desire to gain momentum in your recovery but do not know where to start, this is where I can help. I’ll coach you and help you gain clarity on where you are currently in your recovery journey, I will help you to create a picture of where you would like to be in your recovery 12 months from now, and I will coach you to overcome what’s stopping you from getting to your goal.
Bill 2:27
During coaching, I’ll also teach you the 10 steps to brain health for stroke survivors and guide you through each step with supporting interviews from experts and information that is based on the latest scientific research. If you’re one of the first 10 people to join recovery after show coaching you will get a one-on-one private coaching thread with me access to the course 10 Steps to brain health for stroke survivors when released.
Bill 2:52
Members access only monthly group training calls and access to the stroke survivors’ private forum The first 10 people to join will also get more than 70% off the full price of 599. And 12 months of access will only cost you $149. One of the first 10 people to join recovery after show coaching now and get the first seven days free. After the seven-day free trial, you’ll pay the annual amount of only $149. And the price of renewal will never increase for as many years that you stay a member.
Bill 3:25
Once the first 10 coaching packages are sold, the price will increase and never be offered again. So take advantage of the seven-day free trial now by clicking the link below if you’re watching on YouTube, or by going to recoveryafterstroke.com/coaching if you’re listening online. Now it’s on with the show.
Bill 3:41
Jessica Tagami. Welcome to the podcast.
Jessica Tagami 3:44
Thank you very much for having me.
Bill 3:46
Thank you for being here. I understand that one of your family members has had a stroke. Tell me a little bit about that.
The Symptoms
Jessica Tagami 3:53
In November on the well, it was overnight. So it was between November 11 and November 12, that my husband fell asleep and then woke up and felt like he had slept on his arm funny and he felt like maybe he had lost sensation because he had put all his weight on it overnight. And then a few minutes went by and he had gone, gotten up out of bed and tried to go to the bathroom and realized that he was not getting any of the pins and needles or anything that you would find once you know you start getting circulation back in your arm, and he realized he couldn’t move it at all.
Jessica Tagami 4:41
And so he thought maybe he was having a stroke. He Googled symptoms of why his arm maybe wasn’t moving. And told me he thought he was having a stroke and could I please drive him to the hospital because he was talking fine. Maybe he was a little bit tired, but he had woken up early, it was around 5:30 maybe a quarter to six in the morning.
Jessica Tagami 5:06
Then by the time we got to the ER, he was diagnosed he is having a stroke and he also found out in the same sentence that he had undiagnosed type two diabetes, which probably helped cause it. And then he had a second stroke eight days after that, and the grand mal seizure spent about 21 or 22 days in the hospital, and then came home and it’s been now I think he just passed the 60-day mark a couple of days ago. So you can go into a lot of therapy and try to regain his life back.
Bill 5:48
Wow, what’s your husband’s name?
Jessica Tagami 5:52
Phil.
Bill 5:53
Phil. So how old is Phil?
Jessica Tagami 5:58
54.
Bill 5:59
54. So young. And this thing is you go to bed you wake up in the morning and your lives are changed forever. Not only did Phil’s life change, but we hear from stroke survivors on the podcast all the time how their lives changed. What was different about it after that, You’re an artist and an amazing artist, by the way. I’m looking at your website, JessicaTagamiArt.com we’ll talk about that a little later.
Bill 6:26
But, your role in this family is not a carer of somebody who’s had a stroke, you don’t have any skills, any knowledge. You don’t have any background in being able to support somebody like that. What is it like to go to the hospital and experience this process of learning that your partner, husband, whatever, whatever that person is, your family member has had a stroke?
Jessica Tagami 6:58
Yeah, I think the first thing is that I feel so bad for people
Jessica Tagami 7:07
In this community that nobody wants to be in, but once you’re in, you’re grateful for the support. But people there are a lot of people I think, who are shocked that they had this happen to them, or that they had a family member who had this happen to them. And my husband and I, so we’re talking maybe a month after the fact of how this wasn’t a surprise for either of us. We thought something was coming.
Jessica Tagami 7:38
The fact that it was a stroke was a little weird, but he has a very high-pressure job is under a lot of stress, didn’t take care of himself. And so, that part, the part that feeling shocked wasn’t there, but the crisis mode that comes once the incident has happened, once a stroke has happened. That went on for like a full month when he was most of the time that he was in the hospital. And then for a few weeks after that, just trying to adjust to the new life that we had to build for ourselves as far as new routines and just being mindful of temporary and who knows if there are any permanent limitations.
Jessica Tagami 8:29
I mean, right now, it seems to be hopefully mostly temporary, but it’s still it’s a long process. And yeah, I don’t feel like we, I feel like we’re still learning how to deal with that. That whole process of what do we do now that this is all happened because we have two teenage kids and they’re also processing that I think probably still to this day just kind of I mean, in the way that you know teenagers do, and just trying to, I don’t know, be supportive of my husband but also try to figure out what a new normal looks like, I guess.
Progressive Stroke
Bill 9:19
Yeah. So when Phil came home, what did he come home with any deficits? Was there something physical?
Jessica Tagami 9:26
For sure he had a deficit. So he had you know, I don’t know, you might know better. But I didn’t register with me whether or not there’s a specific name for he had a right brain stroke both times. So it affected the left side of his body. So his left arm had no movement in it. Pretty much the whole time that he was at the hospital, and he just started to get little bits of feeling back maybe a week after it happened.
Jessica Tagami 10:00
Then he had a second stroke. And so was further weakened by that. I would say they called it the first stroke, progressive stroke because when he first day went into the hospital, he got the arm. And then he woke up the next day and was in acute care and said that he felt much better. And that was probably because they were also treating his undiagnosed diabetes, so his blood sugar was getting better managed.
Jessica Tagami 10:32
But then on the third day, after the first stroke, he lost a lot of mobility and strength in his left leg in addition to the left arm, and that freaked him out quite a bit. And then they told him, You know what, it’s not that uncommon for you to have a progressive stroke. It’s just your brain is trying to, you know, you might get further dead tissue, I guess in your brain, and your neural pathways are trying to figure out different ways that they can readjust.
Jessica Tagami 11:09
And then on the eighth day, he had a second stroke he was in, actually, he was in physical therapy at the hospital. They were fitting him for a new wheelchair that was going to have a special armrest for his left arm. And he just remembers he says he remembers seizing like his arm shot up without him being able to control it and then started clenching. And then he had a seizure. He woke up and they took another MRI, took him down to the ICU, and then realized that he had a second. It was like a smaller portion of his brain that was affected, but it was considered a second stroke.
Bill 11:51
Yeah. And was it as a result of a bleed or a blood clot or something else?
Jessica Tagami 11:57
That’s interesting. They were trying to figure out if his heart was throwing off clots, but they still hadn’t quite figured that out. So I think it was a second bleed. But yeah, I’m sorry, I completely birdwalk that last question. I meant to say to you that he came home with both leg and arm deficits when he finally got out of the hospital.
Bill 12:18
Yeah, I got a feeling that that was the case, but that’s okay. So you know, you said he was scared about that I mean, I was scared. It was completely bizarre that your body is doing x, all these things normally in their problem. And then after a certain period, it’s not able to do those things. And you think that you can and you think you’re capable. But there’s a physical disconnection and it just doesn’t do it. And on the left side, my body is numb and it does have deficits and I have different sensations and all that type of thing.
Bill 12:52
And that’s come back online. I’m 8 years down the track and on the right side, my body feels the same as it always did. When I went to the gym for the first time last weekend, in about two or three years, the instructor I said, I explained to the instructor what my issues were when I told him to take it easy on me. And we did this little circuit. And I was doing well. But if I can describe it to you so that you can understand what it’s like from a stroke patient’s perspective, it’s like my left side had done a marathon and my right side was just warming up.
Bill 13:31
My left lung leg. Every part of my left side was completely spent after this hour session and my right side went. Alright, let’s do this.
Jessica Tagami 13:47
Yeah, he says that too. It’s funny that right now he’s trying hard to work on fine motor skills for his left side. But if he tries to pick up a fork a spoon or a pencil. It looks like he can do it. It takes him maybe a full 30 seconds to reach down, pick it up, and bring it back up. But it looks like the grip is soft like it looks like I’m worried that it’s going to fall out of his fingers and he’s going to get frustrated.
Jessica Tagami 14:29
He manages to hold on to it, but then when he puts it back down, he’s sweating. I mean it takes but you know his right side, he’s just like, whatever. Okay, we’re going to pick this up. So yeah, I can see how you would have that feeling on opposite sides of your body and it must feel so strange. I had no idea about that.
Bill 14:35
Like two people in one body. But the same personality.
Behavioral changes
Jessica Tagami 14:53
The personality is interesting. Actually. Do you. Did you find after you had your stroke that there were any not personality differences, but any enhancements or any interesting additions to your personality?
Bill 15:12
Yeah, my wife wouldn’t describe them as interesting, Jessica but I became a bit of a bastard quite nasty. at one point for quite a while it took me I would say the best part of about, you know, 9 to 12 months to calm down and I’m not saying that I knew what I was doing or I was responding purposefully in an angry way, it’s just that something was making me angry quicker, shorter, faster, longer.
Bill 15:45
And it was, yeah, really nasty stuff. You know, I would scream at my wife. Because I was so fatigued. I would scream at her for parking in the wrong parking spot, according to me and it was needed to take the parking spot that was two cars over so I could be you know, five feet closer to the door. And that used to just send me off the deep end.
Bill 16:07
And then I remember one time I was on a steroid that was helping to reduce inflammation in the brain and that steroids was called dexamethasone, and one of the impacts that it had on the body was that it made you hungry. And just to make you feel like your hyperglycemic drop your blood sugar, and then make you eat like just some crazy person. And as a result of that, I put on a lot of weight. And I became in two weeks I put on the equivalent of eight kilos, which I think in pounds, I think it’s like
Jessica Tagami 16:44
About almost 20 pounds right?
Bill 16:46
And yeah, right. within about two weeks, my clothes stopped fitting me I didn’t have any clothes to wear.
Jessica Tagami 16:53
Which is gonna get you angrier right?
Bill 16:58
Yeah wife was sweet and thinking of me when I was complaining about my way, I asked her to buy me some ice cream but she bought me low-fat ice cream.
Jessica Tagami 17:10
Why bother?
Bill 17:12
That’s and it was, it was an email or an SMS rant and she thought at the beginning that I was joking I was dead serious. I was so offended that she bought me low-fat ice cream. So anyhow, I started to become aware of my behavior. And I started to try to address it. But what I noticed another thing I noticed was that I did become a lot more emotional and cry at the drop of a hat.
Bill 17:46
And I also became aware of my emotions. So not only was I emotional, but I became aware that I had emotions like my heart came to life. I found that my head switched off and my heart kind of life. And then what that made me do is be a little bit more caring and conscious of the people around me, although I did make it all about me and trying to heal and recover and all that kind of stuff. I feel like I took no prisoners during that time. And that meant that at the beginning, I was probably a very difficult person to be around for quite a while.
Jessica Tagami 18:26
Did you come to that realization yourself or did you have not behavioral therapist, I mean, I know that stroke victims often get you know, occupational therapists and speech therapists, physical therapists, and neurologists. Did you have other people telling you that or did you come to that realization on your own? The fact that you had to be more aware of your emotions.
Bill 18:50
I didn’t come to it on my own partly, I was probably frustrated about the fact that now that I needed my wife the most I was giving her such a hard time. But one of the first things I did after my first bleed, which was in Feb 2012, was I was in hospital for seven days. And then I immediately made a point to see my psychologist and I had been seeing a psychologist since I was 25. And I was 37. By now. I’ve been seeing the psychologist early on to just be understanding of why we interact with certain people in certain ways, family, friends, work colleagues, and why they respond in certain ways to me, I started to become comfortable with myself and how I interacted with people.
Bill 19:41
Up until then, and then afterward. My understanding of how I was behaving had changed so I needed to learn what was happening to me and the counseling sessions made it possible for me to feel like it was just part of the process, it’s part of the response that my brain is putting out there, my wife came along to some of those sessions I brought her along as well. So that she can understand that I’m not personally attacking her because I hate her or I don’t like her or (inaudible).
Bill 20:18
It’s just because something’s happening to me that I don’t know that there’s an imbalance and I’m not sure how to fix it. So that helped. And then I’ve continued my coaching journey with other people who are not psychologists to worry more about coaches who support people to overcome frustrations, of the lack of doing something so more about me being proactive in taking action to achieve those little things that I enjoy in my life.
Bill 20:51
And then as a result of that, I started to address all of these underlying issues that come up to the surface, just when you’re in the worst time of your life dealing with stroke that you had all suppressed, or you had buried under the carpet. And now they’re going, Hey, you haven’t been paying attention to all these things. By the way, I know you’ve got this brain thing that you got to deal with, but have a deal with all this stuff as well.
Bill 21:15
It becomes overwhelming. And sometimes, I’ve had people that I’ve interviewed through the podcast, I’ve said stuff like, I dealt with all of my physical issues for 20 years, and I’ve never dealt with my emotional issues, and they’ve just started the journey later. So if you can have that awareness together early on, it’s and then slowly sort of formulate a little program to deal with everything. as it appears or as it turns up, then the emotional side of it gets dealt with and then we can get clear on the physical side of it because for me the emotional side, if I get emotional, action, clarity, all that stuff disappears. But if I deal with my underlying emotions I can get really clear on my outcomes, my goals, my achievements, and the things that I want to overcome.
Recovery could be a lifelong journey
Jessica Tagami 22:09
Right. Now that sounds that sounds fair. Yeah, we’re dealing with all that right now too in real time So, so eight years down the road, you’re still dealing with that.
Bill 22:20
Yeah, I hate to be. I hate to be the guy that says it’s gonna be a lifelong journey.
Jessica Tagami 22:28
Yeah, no, that’s fine.
Bill 22:31
It is and it’s not because it’s because it’s very different in the brain. It’s not like a finger, you cut it and then the finger gets better and then you just move on with your life in the brain. The healing takes longer firstly, so you might, you know, it’s not uncommon to hear people from the medical community say stuff like, you know, give it two years or three years or six months or 12 months. They never talk about giving it days or weeks. They always talk about long periods.
Bill 23:00
Especially with neurological deficits, mine all came all went away after the first two brain bleeds, so I got to the point where I didn’t know my wife, I got to the point where I didn’t know who I was what was happening, or that type of thing. I couldn’t speak, make a sentence, finish a sentence, remember who visited me, all those things I couldn’t do. And then all of those things came back online over about three years. Just as everything was coming good. I had the third bleed and had to have surgery and that surgery was what created the deficits that I’ve now had for five years.
Intro 23:43
If you’ve had a stroke, and you’re in recovery, you’ll know what a scary and confusing time it can be. You’re likely to have a lot of questions going through your mind. Like, how long will it take to recover? Will I recover? What things should I avoid in case I make matters worse, doctors will explain things. But, because you’ve never had a stroke before, you probably don’t know what questions to ask. If this is you, you may miss out on doing things that could help speed up your recovery.
Intro 24:13
If you find yourself in that situation, stop worrying, and head to recoveryafterstroke.com, where you can download a guide that will help you. It’s called seven questions to ask your doctor about your stroke. These seven questions are the ones Bill wished he’d asked when he was recovering from a stroke. They’ll not only help you better understand your condition. They’ll help you take a more active role in your recovery. Head to the website now, recoveryafterstroke.com, and download the guide it’s free.
Bill 24:55
So those deficits meant that I had to learn how to walk again and use my left arm again I started to learn how to use them in a walk with these altered versions of my left side with this altered version. So then what happens is you start to grow accustomed to this new version of yourself. And I’ve got this great tool now for telling me how well or unwell I am and how tired or, or fresh I am, and that’s all my left side because when it fatigues it’s usually a sign for me to rest.
Bill 25:33
Even though the rest of my body is going it’s all good. The left sides going, you’ve got to rest and I know that I’ve just had to sit down, get off the computer, and do nothing. So I started to become good at reading the signs from my body, which I never was before. I was oblivious to the feedback that my body was giving me.
Jessica Tagami 25:54
Okay, how often do you go to therapies or sessions to work on your deficits and improve them?
Bill 26:06
Yeah, when I was first out of surgery, I was going three times a week for months. Hmm. And there were different therapies. So one might be hand therapy. The other one was foot therapy. And we would go on a week, they would go on a Tuesday, Thursday, and a Friday. And each session would be about an hour. And at the beginning that felt like there were about a year’s worth of, you know, if it was just so difficult.
Bill 26:39
And then as time went on, I started to get to the point where I started to feel comfortable. And I had this amazing therapist who said to me, like, what would you like to get back or do or achieve while you’re here? And one of the things I wanted to do was run across the road. So to get away from a car if there was a car coming.
Jessica Tagami 26:58
Yeah, that’s a good thing to know and be able to do.
Bill 27:02
And that’s what we worked on. And he was able to record me running and show me some footage of me running so that I could get an understanding of how I was doing it. About three or four months later, I got to that point where I still needed therapy, and I didn’t feel like I was completely done. But it was enough to be able to say to the guys nicely, I said to him, You guys are sacked. I don’t need you anymore.
Bill 27:27
And thank you, you’ve done a great job. And I’m going to take responsibility now for my therapy. And that involved going to the gym. When I got my balance back, I started to ride my bike again. But I started to do it in a very different way, in a way where I needed to strap my foot onto the pedal because I didn’t realize I couldn’t feel the pedal so it kept falling off and slipping off. So I did all these little things so the therapy continued and just evolved into things that I liked and enjoyed doing and it started to include walking and all sorts of other things.
Bill 28:05
And then what happens is you start to feel like you’re achieving something and you start to get comfortable with how the body is progressing, and how the differences affecting you. It starts to become a new normal and people talk about a new normal, but you never know what that is. It’s always evolving and always changing. And especially when you’re early on in the process, like you guys are, continue to evolve and change. They’ll be very, very many ways that people train and adapt.
Jessica Tagami 28:43
Yeah, it’s interesting. We’ll see. I mean, I feel like he’s making a lot of progress. It’s funny that you said that thing about the taking years. That’s the way that therapists and doctors talk when they’re talking stroke victims because the main deadline that we’ve been hearing, even though they do say it’s going to take a long time, it’s going to take years for, you know, for you to get everything back if that is in the cards for you.
Jessica Tagami 29:14
They kept focusing on a 90-day thing, I think because they wanted him to make sure that he was moving, you know, his shoulder joints, making sure that muscles weren’t, atrophying. So my husband has been very focused on the whole 90-day mark, being able to see if he can get the range of motion, obviously not the strength back then he’s been working on that.
The 90-day stroke recovery period
Bill 29:43
So the doctors will give you those 90 days because there’s a critical time in their thinking about when the most recovery occurs, and it happens in those 90 days. So what they say and unfortunately, sometimes they negatively use that and I don’t like the way they use it. Sometimes they say, Well if you don’t get This back in the next 90 days, it probably won’t get it back at all.
Bill 30:03
But what I hear from the people that I’ve interviewed and from the people in the community is that very often, many of them are getting function back and movement back in and now that wasn’t working for 10 years or 20 years. So this comment that they make is a little bit difficult for me to hear. And people need to know that there’s no such thing as never if you’ve got time, anything is possible.
Bill 30:35
So what you hear though, is that in that 90-day window, the most recovery will occur. They want you to take advantage of their time because the brain rewires itself and it’s creating new pathways and in that time you’re creating neuroplasticity, and neuroplasticity requires ongoing repetitive tasks. So that the rewiring can occur as quickly as possible. And then once it’s cemented, it keeps going.
Bill 31:04
So they talk about that as the right time to take the opportunity to do as much rehab as possible to rewire the brain as early as possible. There is such a thing as negative neuroplasticity as well. And that’s when people take tasks that they don’t do so well. So you might find that sometimes there’ll be some people who have learned how to walk, again, with their cane or their walker or their device that helps them walk, and then for some reason, out of fear, perhaps they haven’t let it go.
Bill 31:45
And they may be making a really good recovery, but in 12 months, they’re still using their walker. Right, altered their entire gait, and it’s altered everything about the way that they walk because now they lean forward slightly and their balance is out and the center of gravity is out. And all these things occur. And then to get them back to walking the way that were before, you have to train them out of the the new pathways that were created walking with this walker that have been cemented in.
Bill 32:18
So the 90-day period is important. But then the ongoing period is also important because you don’t want to be doing something in 12 months that you don’t need to be doing, that you had to do at the beginning just to get you on your feet and get you up. And you know, so doctors will throw the most resources, the most rehabilitation will happen in the first 90 days.
Bill 32:44
And then they will say, Well, you’ve achieved or reached a certain point, and that’s as far as we could take it and then you’re on your own. And the important thing to realize when people come home is that the rehabilitation doesn’t stop even though you’re not going to. Formal rehabilitation needs to continue.
Jessica Tagami 33:05
Yeah, I’m sure that that’s also a failing of I don’t know how your healthcare system is. But I mean, I’m sure that they’re going to try to push my husband now as soon as possible so they can stop paying for therapies. So be interesting to see what happens after a certain number of days.
Bill 33:24
Yeah, it’s the same, same here. There are so many people waiting to get into beds because, unfortunately, the number of people having a stroke is increasing. I think the stats now are one in four people will experience a stroke in their lifetime.
Jessica Tagami 33:40
No kidding, wow.
Bill 33:41
So they need the bed. So the sooner they can get people out of the bed, or out of the service, then they’ll get them out of there. And it’s a challenge. It’s, it’s a life-threatening challenge. It’s a health challenge that has a long lifespan. It’s not like breaking a leg, you put it in a cast, and it gets better when you back to normal, Unfortunately, high resources require people to get back on their feet back to work. And that’s why they will push you out as quickly as they can because they need to make space for other people.
Jessica Tagami 34:21
So were all of the bleeds that you had, did they diagnosed them as separate strokes, or were some of them labeled aneurysms?
Bill 34:33
So my bleeding was caused by a faulty blood vessel, and it was there from birth. And what happened was, it’s interesting that you said that you guys weren’t shocked that your husband had a stroke that Phil had the stroke that it was kind of made kind of logical conclusion to how he was perhaps being in his life. Well, I created the perfect storm for this thing to bleed as well as how I describe it and it bled at the same spot three times the first time it bled a small amount.
Bill 35:04
The second time it bled a larger amount, the blood clot was about the size of a golf ball. And then the third time it bled a smaller amount than that. And then they said that look, we’ve got to get this out. We can’t leave it there because it’s becoming dangerous to your health and well-being. So they removed it, I was taken, and I was picked up when you said that it was a logical conclusion that something went wrong. Does Phil see that in hindsight?
Jessica Tagami 35:38
Oh yeah, absolutely. We had several discussions because the TV was bad in the hospital, so we definitely and you know, he was feeling his mortality. And so we had discussions about that sort of subject matter. And he knew it. I mean, he was surprised, And then in the same instant not surprised that he had been diagnosed with diabetes as soon as he got into the hospital because he had felt like crap for months.
Jessica Tagami 36:13
I mean kind of a year he had felt like crap, you’d always attributed it to the high stress levels that he was feeling from his workplace. And so he just thought that because he was working long hours, and eating a lot of restaurant food, because he was doing a lot of meetings over dinner, and then coming home and taking a long time to unwind because he needed to process his whole work day.
Jessica Tagami 36:43
And so maybe only averaged five hours of sleep if he was lucky. He thought that that was all why he was feeling so bad. But obviously, his body was just also poisoned because of the blood sugar levels and so we talked about in the hospital, about how that and the stress levels and just because he was working such long days, he would make promises to himself that he needed to take better care of himself by going to the gym regularly.
Jessica Tagami 37:16
But that never happened. Because you know, another meeting would come up or somebody else would need his time or need him to go on a conference call so things just would pop up every single time and the prior he prioritized work because he just wanted to get certain things done. And it almost killed him when the end so yeah, no, in hindsight, he realized that it wasn’t surprising that something happened.
Jessica Tagami 37:46
I don’t know if he would have predicted a stroke. I think he probably would’ve, because of the stress he might have, you know, people automatically go to the idea of oh, God that person is somewhat stressed, you know, a perfect candidate for a heart attack, but instead, it was a stroke.
Bill 38:02
Yeah, so it’s interesting that you said the thing that you did about sleep now as he is overweight. Would you have considered him to be overweight?
Jessica Tagami 38:11
He was overweight and he still is but he’s lost. So I don’t know sorry I don’t know the centimeters but he’s about five foot nine. So I don’t know if you can.
Bill 38:25
It’s about 180 centimeters or something.
Jessica Tagami 38:28
So he’s about that and he knows you’re gonna have to translate kilos cuz he’s about he go into the emergency room at about 273 so quite a bit overweight. And he lost nearly 30 pounds since the stroke happened because he’s had to change his entire diet for diabetes. But as I said before, just eating restaurant food which is full of salt and butter and all that delicious stuff is terrible for you.
Jessica Tagami 38:59
And you know, having a couple of glasses of wine over dinner, it just all added up, and not exercising. So was overweight. Before he got that overweight though he actually, my kids are 14 and 16 now, but when they were, like two and just born, he was having trouble sleeping and ended up going to a sleep clinic and got diagnosed with sleep apnea. So he was one of those Darth Vader machines and practically since I’ve known him, he’s been doing that for at least 16 17 18 years.
Bill 39:39
Yeah. Wow. So I’m 273 pounds 123 kilos, and that’s quite heavy for somebody who’s had, you know, five foot nine. Yeah. So what’s interesting is that people may not realize that when you are somebody who sleeps a low amount of hours. The way that your body metabolizes sugar completely changes. And the white chain in somebody is more likely in somebody who sleeps less than your standard eight hours a day. As a result, people who sleep less are far more likely to have diabetes type two diabetes.
Jessica Tagami 40:24
And I also have, I mean, we had read just because he knew that he was under stress, he had researched a lot about what stress does to your body and the cortisol that releases and how that also messes your sugar levels. So yeah, he was in hindsight, it’s he was It’s actually, the only surprise that he didn’t get it sooner. But he’s a pretty strong guy. So I think that’s just why he was able to tolerate as much as he could.
Bill 40:55
“Tolerate” is one of the keywords I think. Absolutely the amount that people tolerate is just ridiculous even in personal relationships, and you know, physical pain and all sorts of things. People just tolerate stuff and they become immune to issues and challenges and they kind of make it well, that’s normal for me. Like, I’m always like that. I always feel like that. So I didn’t see anything different.
Bill 41:21
It’s not normal to be in pain all the time not get enough sleep or not breathe properly when you’re sleeping. That’s not normal. So it’s feeling like they’re tolerating a whole heap of stuff and they think that it’s their normal. Ask somebody else if they’re going through the same thing, because if they don’t tolerate as much pain as you do, then maybe it’s not normal for you. Maybe you need to look into it and do something about it.
About Diabetes
Jessica Tagami 41:46
Yeah, it’s interesting that you say that because the first day that we were in the hospital, we were still in the emergency room and they were waiting to bring them up to bed. And, the emergency room nurse just could not believe it. So I don’t know. Do you know anything about diabetes? Because I’ve learned a whole lot in these last couple of months.
Bill 42:07
I know a little bit about diabetes tell me.
Jessica Tagami 42:10
So I had no idea what normal blood sugar levels were only because it’s never been an issue before. But you’re supposed to be in this safe range, which is the love for you to be, like, around 100 to 120 150 is like the very limit. And when they took his blood sugar when he went into the emergency room, it was at 611.
Jessica Tagami 42:35
And the nurses just kept coming up to him and they just kind of feel like Didn’t you just mean how did you not know that you had this this high of a blood sugar level? No, didn’t you feel bad? And he’s like, I was just used to it. So it’s kind of yeah, what you just said, what you tolerate and how you feel like it’s, this is normal for me, but it’s just for somebody else. It’s terrible.
Bill 43:00
Yeah, ask other people if you’re missing a leg and you had it in the morning, and you look down and you’ve gotten a leg, and now you’re hopping to work because you got to get to work. Just ask, ask somebody somebody like, did your leg just drop off out of nowhere? I gotta get to work because I gotta pay the bills. I’m going to, you know, put food on the table, I’ve got to do all those things like I get it that was me that was how I used to talk to everybody about it, everything, you know, six, seven days a week, I would work if I had to if I could.
Bill 43:30
If I was allowed to my wife let me I would. So it’s a bit of a thing that we get stuck on and it doesn’t happen immediately. It kind of is a process that creeps up on you and sneaks up on you. And you go well how did I get here but it feels years. Slow, small steps to get there. Tell me about whether was it scary for you to go through this process how did you feel when you knew, or discovered that your husband was experiencing this life-threatening issue and now is in hospital work what was that feeling like?
Jessica Tagami 44:12
um, the first day was interesting because he was kind of in good spirits even though he seemed sleepy and his leg and his arm weren’t working the first day when he was in the emergency room he was making jokes and just was kind of tired but he wasn’t slurring until the third day. And he didn’t, you know, it didn’t have any memory loss or anything. So when I had spent a little time with him, driving him to the hospital and listening to him. I didn’t get really scared because I felt like okay, this was the thing that I was thinking was going to happen because we haven’t been taking care of him, and thank God it wasn’t a heart attack.
Jessica Tagami 45:02
This may be this is a stroke or whatever this is, but he seems like it didn’t seem life-threatening to me, It was only on the eighth day when he had his second stroke, and they called the Code Blue. And, you know, rushed him into the ICU from the physical therapy room that I started to get scared, and that’s when I panicked, but for that first week, it was more of visiting him and closely monitoring, you know, because he had a little bit of a progression with his leg on the third day, just kind of seeing what was going to happen and but I felt reassured because the doctor said, you know, this is not, you know, uncommon, and she’s going to take a while, but we feel like he’ll be fine eventually he’ll be fine.
Jessica Tagami 45:55
And so once you hear that, you know, you just work toward that goal, right? But then when the second stroke happened, and we were already in the hospital, and you felt like you were doing everything right, and you’re supposed to be in the safest place that you’re that you could be in something terrible like that still happens. That’s when we, I think a lot of us got scared. But so I would say the whole time that he was in the hospital because he had been diagnosed with diabetes, he was on a strict diet. Unfortunately, the hospital had the week before to change their catering, food, and food prep. They were still working out stuff so they just could not wrap their head.
Bill 46:53
That’s cool.
Jessica Tagami 46:55
They couldn’t wrap their heads around the idea that he was on a very restricted diet. And so I ended up bringing him all his meals. And that was a little challenging, but fortunately, we’re only about four miles away from the hospital. So, but it was you know, I was just kind of a robot for the first month while he was in the hospital because I had to make sure that the kids went to school and got picked up from school.
Jessica Tagami 47:20
Make sure he gets all his meals. There was a period in the first week I want to say where it was after actually, I know when it was it was right after he woke up and lost a lot of mobility in his leg on the third day that he might have panicked a little and so he asked me to stay with him for a couple of nights. So I would you know, come back make sure that the kids had dinner and then you know, go back to the hospital and then stay with him for the night.
Jessica Tagami 47:51
And in between all that this is kind of funny now but in between all that he had his car stolen from the hospital parking lot. And my car got rear-ended when I was on my way to the hospital. So there were some driving challenges for me for a week getting to and from a hospital but I would say when we got home from the hospital, I mean I just kind of felt relief that he was home and then he was able to be home without having I know that there are some people who come home and they still need to have at least part-time like home health aides.
Jessica Tagami 48:33
I think home health care aides come to help them with you know if they need to take a shower or you know, some people just aren’t able to do that. And he was he did it very slowly at first. But just feeling I think relief and then just to also been adjusting, which we’re still doing adjusting to new routines and the frustration that he can feel when he gets fatigued especially so at the end that It’s so funny that you mentioned it in the beginning about how you got very angry for some time and you didn’t necessarily know that you were feeling emotional or angry, particularly to the people that you know, helped you.
Jessica Tagami 49:22
You felt like you wanted the most help from he asked me this morning because I was driving him to an appointment whether or not I noticed that he was more cranky since this all happened. And I said is, he’s fine in the morning at night, he’s a different kind of cranky because before the stroke happens, he would be so stressed out by whatever was happening at work that he would come home and just not want to speak just kind of wants to either sit in front of the computer screen and mindlessly scroll through Twitter or whatever or, you know, play a video game or watch a movie and just not speak, kind of decompress that way.
Jessica Tagami 50:10
And now, he comes home a lot earlier than he’s back at work, but he comes home a lot earlier and he if he’s tired, he is cranky, but it’s a different kind of cranky where he’s very verbal and just wants to, you know, complain to somebody. And it’s not that he’s mad at me or cranky with me, but he just wants to complain about whatever happened during the day or how he, you know, felt like somebody treated him differently because of the deficits that he knows that he felt was unfair because he doesn’t feel like he doesn’t feel different, except for physical limitations.
Jessica Tagami 50:53
But he feels like a lot of people are wondering whether or not he has mental limitations. And so they’re questioning his judgment at work. And that’s very frustrating to him. So I kind of absorbed that for him at the end of the day, if he wants to vent, that’s fine. But that’s kind of what we’re dealing with now.
Becoming more compassionate after experiencing a stroke
Bill 51:16
Isn’t it amazing? You’ve been healthy one day and the next day you can relate to all those people that have been discriminated against.
Jessica Tagami 51:24
He says that that’s so funny that you say that he’s noticed that a lot and he’s vocalized. But he’s like, I used to never pay attention to people who are walking with a cane or who needed extra time to cross the street and now that’s all he sees.
Bill 51:38
Stroke has this way of making people more compassionate. It’s a shit way to get too compassionate. But it does do that. Tell me about the conversations that you had with the girls or with the teens. I don’t even know if the girls or boys.
Jessica Tagami 51:56
One boy one girl yeah.
Bill 51:57
How did the conversation go with your kids?
Jessica Tagami 52:00
That’s interesting. I don’t remember. Because honestly, that month was a blur. I mean, so he went into the hospital on the first day at like seven o’clock in the morning, I think. You know what it was? And I said, kids, I can’t take you to school, they stayed home from school that day. And so I just texted with them throughout the day saying, he’s fine you know, we’re going and he has had this happen to him, and he’s been diagnosed with this and we’re waiting for a room, but it’s going to be okay. And I’ll come home sometime this afternoon and make sure that you can come see him.
Jessica Tagami 52:43
Then they were you can see that they were a little panicked when I did pick them up when I took them to the hospital and they saw that he was joking the first day I think they relaxed a lot. And they’re aware of the fact that he was under high stress and didn’t take care of himself. So I think on some level less than me. They also were not entirely surprised, you know, upset but not entirely surprised that this happened to and when they saw that he was able to speak and joke that made them feel better.
Jessica Tagami 53:16
I think they like me had that day of panic when he went into ICU and they wanted to see him right away. So I took them out of school early so that they could come see him. But since then, I think I think it wouldn’t be different if a stroke had affected more of his memory or verbal cues or verbal abilities, but it hasn’t. He can speak just as quickly and with complexity, and so you know, he just imparts his dad wisdom on them and tells bad Dad jokes and they roll their eyes at him and, you know, they’re pretty resilient.
Jessica Tagami 54:07
I think so but I think it would have been for all of us it would be a lot more emotionally frustrating, worrying, if he wasn’t able to communicate with us and tell us his needs, you know, he’s able to say, hey, I need help. I can’t carry this bag up the stairs. Can you help us But imagine, you know, I can’t imagine being, a stroke victim who can express what they need or communicate what they need. That would be terrifying.
Bill 54:38
Yeah, there is a very broad range of the impact that stroke causes on survivors and then on families. Everyone’s different so everyone responds differently. Children respond differently. My children took it in their stride mostly. But I dragged them to therapy with me.
Jessica Tagami 55:00
How old are they now?
Bill 55:01
They’re 23 and 19. Now, so that eight years ago, you know, they were 15 and 12 I think, somewhere there.
Jessica Tagami 55:14
Roughly the same age that mine are too. Yeah, 14 and 16.
Bill 55:18
They do bounce back their quite resilient, but I feel like my youngest had a lot more stuff that was unresolved for a longer period. And that impacted on him and he wasn’t aware of how it was impacting on him. And he’s a lot better now. And we’re all a lot better now. Because so much time has elapsed, I’m staying proactive in the things that I do to overcome a stroke and to learn about stroke or to share about stroke. So they’re seeing me doing that and that kind of makes everything okay now and better. But, they were going for one of them was going through I think it was when I went to surgery he was going through the last year of school, exams and all that kind of stuff. So that was extremely difficult for him.
Bill 56:14
And then at the same time, I had surgery in November 2014. I think it was two weeks earlier, that my mother-in-law passed away.
Jessica Tagami 56:24
That’s terrible.
Bill 56:24
So I had just had the third bleed getting ready for surgery, and she passed away a week and a bit before my surgery. And it was just horrific. You can imagine everyone going through all the emotional turmoil of stroke and then, you know, throw that into the mix and somehow try to talk to kids about I’m going to be surgery tomorrow and it’s a life-threatening surgery, etc. You know, so it’s a real tough time.
Jessica Tagami 56:51
I’m sure and for your wife too I’m sure,
Bill 56:53
Yeah, she’s just and that’s the reason why I’m interested in hearing from wives is to understand a little bit better about my wife because I haven’t interviewed her yet. I might do it for the hundredth episode. I’ve been thinking and I don’t know if I’ll be able to get through it though, Jessica.
Jessica Tagami 57:17
Maybe you should have a guest host then.
Bill 57:19
Yeah, maybe they can interview both of us instead. Maybe you can interview us? What do you reckon? So, yeah, so it’s a very interesting thing, and it’s thrown on inexperienced people, You’re not a doctor, you’re not a nurse. You’re not a health care provider, you’re just a regular person going about your daily tasks, Then you have to become an expert in this field, which is so complex and so challenging, and so emotional, you know, uncharted waters.
Jessica Tagami 57:57
Oh, yeah.
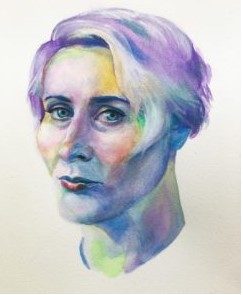
Jessica’s art therapy
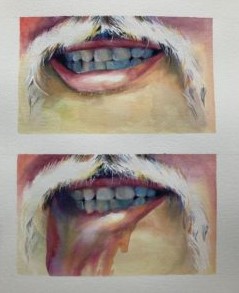
Bill 57:58
So I appreciate hearing your version of the story now, I became fascinated when I saw one of the images that you posted on Instagram, which was a picture of your husband and his face with the lip before and then the lip how he described that at it looks like the liquid washed away and I’ll make this image available if that’s okay with you on the video feed. So how good is it to be able to use art to express these things? Is that something that helps you does it serve you?
Jessica Tagami 58:39
You know it does. It’s interesting I’ve never actually been a person who enjoys some people like to do art as a means of expressing their emotions and for me, it’s always just been meditative So, but once he had the stroke there were a lot of emotions that I was feeling that I didn’t feel I could express in the moment because I felt like I needed to be more compassionate I think.
Jessica Tagami 59:27
My husband will tell you my go-to response if somebody lashes out is for me to probably say something rather than bite back and I couldn’t do that with him because I knew that when he was tired and when he was no probably feeling scared, frustrated, feeling angry listening to people tell him that you know, he wasn’t gonna be able to do certain things or be a certain way anymore. He would then, either talk to me about that and express anger or, you know how sometimes when you get angry at something, you then take it out on somebody else, even though you know or just, you’re nasty, and you’re not necessarily st calling people nasty things, but you are just not pleasant to be around.
Jessica Tagami 1:00:33
So I was experiencing that but also unable to retaliate. And so for me using my husband as an art subject and trying to express what he was going through was therapeutic because it kind of put me in his headspace and made me understand a little more of what he was going through. And that’s not necessarily something that I would do. But I felt like if I wanted to, you know, have a marriage that would make it through this, then I needed. I needed some sort of therapy and art therapy was what I chose for myself, I guess, in a way.
Bill 1:01:23
Beautiful I mean, talk about having something that you’ve grown to enjoy and love doing just regularly. How you express yourself in other ways for other reasons. Now you get to use that skill to somehow moderate or manage emotions that are coming up and I’ve never heard that said by somebody else, what you said about how you couldn’t retaliate. I mean, that would be so potentially disempowering to be in an argument with somebody because yourself empathetic to their condition. You choose not to retaliate.
Jessica Tagami 1:02:04
Yeah, you can’t. I mean, you could I guess, but then you’re either going to say something so painful and unfair, or you’re just gonna bicker. Do you want your exchanges with this person who you know, is feeling scared or is feeling frustrated? And you just want to bicker with them just because you’re also tired. And you’re also frustrated, because this was not in your plan, either to have this be such a huge part of your life. But now you both have to live with it. And so either figure out a way to channel what you’re absorbing from this person or throw it back at them and then it never ends. So yeah, you got to figure something out.
Bill 1:02:50
Sounds like you’ve, taken responsibility for your own emotions and how you’re going to express them manage them, and deal with them.
Jessica Tagami 1:02:57
Yeah. Thank you.
Bill 1:03:00
We get there we do we grow up and eventually something ticks one day. And we start to take responsibility for our behavior. And we realize we can’t respond a different way. Sure, it’s because my husband’s on the other side of the bed, and he’s just recovering from a stroke. Sure. that had to happen for me to realize that I had a different option. But, I’ve got there I realized that.
Jessica Tagami 1:03:26
Exactly. So I’m having fun with that. I mean, I can’t do it. It’s also I didn’t have to take a break and draw some stupid stuff in between because, you know, each time I finished something it’s, it’s sad to look at you know, what he went through to sometimes and so you just want to go do something that you know, is goofy or that is different, you know, different not solely focused on his pain or his journey. And the frustrating days because they happen quite a bit.
Bill 1:04:04
Yeah, the most recent post or thread, the most recent post, one of them is a dog black dog. Is that one of your dogs?
Jessica Tagami 1:04:13
No, it was my college roommate. She checked in on me when he was in the hospital and we just started chatting. And I said, Hey, listen, I need something. Once you give me a picture of your dog, I know you love your dog, and I need to draw something that you know or take my mind off the fact that this is all going on. And so she had sent it to me and I kind of forgot about it because then I started drawing pictures of him and his recovery. And then I needed to take a break and I just did the dog. And it was fun. It kind of made me smile because the dog is cute, and then I went back to doing another painting of him.
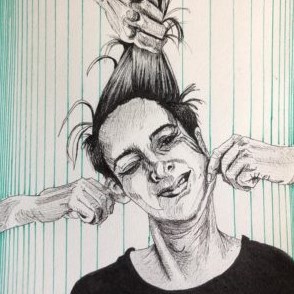
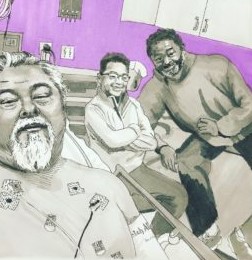
Phil’s portrait as a representation of his stroke experience
Bill 1:05:00
Yeah, I’m looking at those paintings, the painting of the last image of the painting of your husband when he’s kind of side on. And then the dog looks like photos to me. I was gonna ask you are they photos or are they drawn? But they are both drawn or painted.
Jessica Tagami 1:05:18
Yeah. Thank you. Yeah.
Bill 1:05:21
They are amazing. And then on the other side, there’s a photo of him forefront looking as if he’s looking at you, hair is all wavy. His beard’s a little bit all over the place. And there’s a bit of static in the background, what seems like static in the background.
Jessica Tagami 1:05:37
If you zoom in on that, it’s all made with squiggle lines, because I was trying to describe he was trying to describe to me what it felt like when he had the seizure and how he felt like his whole body was being electrocuted. So that’s basically what that picture is.
Bill 1:05:52
Wow, that’s amazing. That is an amazing thing to see in an image because I felt those things as well as I had, and I was not able to express them. The way that I would describe what happened to me at one point when I was going through one of the procedures in the first seven days was like, fireworks were going off in my head, and my eyes, and nobody else could see them.
Jessica Tagami 1:06:19
Yeah, that would be scary. Yeah, I can’t even imagine. Now I wanna draw that I want to draw fireworks that would be amazing.
Bill 1:06:29
Please do please do draw that. I would love to see what your perception of that might be. Because I wouldn’t even be able to describe it. I’m lying there. There’s a whole bunch of stuff going on on top of me, you know, the big surgery, lights, and all that kind of stuff. I’m in theater and they’re doing a procedure where they’re putting a catheter inside my vein in my groin, to take it up to the brain to check out the brain. And it’s freezing and the doctors talking to me and I’m awake and there’s a whole bunch of other people in the background doing their things, nurses, and probably about 10 people around there.
Jessica Tagami 1:07:06
Why do you have to be awake? I’m sorry to interrupt, but why were you awake for that?
Bill 1:07:11
To make sure that they haven’t touched anything they shouldn’t touch? They’re talking to you at the same time to confirm that you’re still responding correctly and the way they want to respond to make sure they haven’t gone to the wrong place. So it’s all done under massive X-ray, and there’s machines and monitors and they can see roughly you know, where they are in the vein and they follow it up through the leg and I pass the heart up into the neck, and then into the brain.
Bill 1:07:44
It’s called an angiograph. And then what happens is these lights you can imagine a theater light how bright it is for them to see it’s like, sun in there. This all goes away. I can’t see anything. It just all goes Black and then all I see is these fireworks things happening inside my eye. My wife asked me how it went, I started crying, it impacted me so much. That’s all I could do was cry. So to see that image, and now for you to explain to me that it was drawn with squiggly lines because that’s how he felt that is an amazing thing to look at is moving for me. I love that. He’s such a beautiful man. He has such something going on about you’ve captured him amazingly well there and I’ve never met him before seen as a regular photo of him, but it just seems like a really powerful, strong man. And I hope you like it.
Jessica Tagami 1:08:46
No, he is. I mean, I don’t think he would have survived how you know, his body was poisoning itself. Unless he was strong. So yeah.
Bill 1:09:00
Well, it has been just an amazing experience getting to chat with you a little bit about your experience of what you went through. I appreciate you sharing that. And I contacted you in the hope that other carers might be listening so that if they are listening, they can potentially relate to some of that stuff and not feel alone understand their frustrations, and then not be able to respond in an argument or bite back is just the way that it goes for a little while. It gets to the point where you’ll be able to bite back at some point but maybe not at the beginning.
Jessica Tagami 1:09:39
I’m waiting for that day.
Bill 1:09:43
Thank you so much for agreeing to be on the podcast and for the art that you do.
Jessica Tagami 1:09:49
My pleasure. I’m going to I’m going to poach one of your pictures from your Instagram account and see if I can do the fireworks thing now because that’s fascinating to me. I love that idea. I mean, I don’t Love that it happened to you. But I love the idea. So thank you.
Bill 1:10:03
You’re welcome, please do. I look forward to seeing what else it is that you do. Before I go, I just wanted to let you know I just completed a webinar about fatigue and three things that people can do to improve fatigue after a stroke. And it was a couple of days ago, it’s being edited now. Anyone who’s listening and wants to get a copy of the video link can get in touch with me at [email protected] but I will make the link available to you so you can have a bit of a watch. If you feel like it and maybe if your husband’s interested, he can have a bit of a look at it.
Jessica Tagami 1:10:39
That would be great.
Bill 1:10:41
Yeah, so just some things to consider that he might not have been aware of. And if he’s feeling tired and needs to sleep, the most important thing for him right now to do is sleep as much as he possibly can. And beyond five hours would be fantastic. If he needs to have a cat nap at lunchtime.
Jessica Tagami 1:11:00
He’s averaging about like seven and a half maybe now, so way better. But yeah, you probably could stand a little bit more.
Bill 1:11:06
Yeah, that is good. Jessica, if people wanted to find out more about the stuff that you do, where should they go?
Jessica Tagami 1:11:13
Oh, well, I don’t do Facebook so if they want to do Instagram, they can go to jessicatagamiart, and they can also go to my website, although I do need to update it is jessicatagamiart.com
Bill 1:11:27
Fantastic. Thanks so much for being on the podcast.
Jessica Tagami 1:11:30
Thank you for having me.
Intro 1:11:31
Discover how to support your recovery after a stroke. Go to recoveryafterstroke.com






